University certificate
The world's largest faculty of nursing”
Introduction to the Program
Mediante esta Postgraduate diploma 100% online, reconocerás de manera temprana los signos de las complicaciones en las Lesiones Cutáneas, permitiendo intervenciones más rápidas”

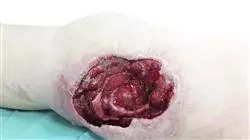
Un informe publicado por la Organización Mundial de la Salud estima que aproximadamente el 15% de los pacientes hospitalizados y el 70% de los usuarios en cuidados desarrollan Úlceras por Presión en algún momento des u estancia. Estas lesiones no solo prolongan la hospitalización y aumentan los costos de atención médica, sino que también pueden llevar a complicaciones graves como infecciones sistémicas y deterioro funcional. Por esto, el manejo efectivo de estas afecciones requiere un enfoque integral, que incluya la evaluación sistemática del riesgo, estrategias preventivas robustas y tratamientos basados en la evidencia científica.
En este contexto, TECH implementa un pionero Postgraduate diploma en Dependency-Related Skin Lesions . El itinerario académico ahondará en la evaluación de las Heridas de la Piel, lo que permitirá a los profesionales diagnosticar correctamente las lesiones que presentan los pacientes y determinarán con inmediatez los tratamientos más apropiados. Asimismo, el temario profundizará en las terapias más avanzadas para los cuidados de las heridas, entre los que destacan la Terapia de Presión Negativo, el Oxígeno Hiperbárico o la Terapia con Láser. Por otro lado, los materiales didácticos ahondarán en la limpieza de las Lesiones Cutáneas asociadas con la Dependencia. De este modo, los egresados eliminarán los microorganismos patógenos y reducirán el riesgo de infección en las heridas.
Por otra parte, en lo que respecta a la metodología, la titulación se imparte de forma 100% online, otorgándoles a los enfermos la oportunidad de acceder al contenido desde cualquier lugar y en cualquier momento, adaptando el estudio a sus horarios. En adición, TECH emplea su revolucionario método de aprendizaje: el Relearning. Este sistema consiste en la repetición de conceptos clave para fijar conocimientos y facilitar un aprendizaje duradero. Además, el programa contará con la participación de un reconocido Director Invitado Internacional, que ofrecerá diversas clases magistrales para ahondar en los últimos avances el tratamiento de Lesiones Cutáneas relacionadas con la Dependencia.
Un reconocido Director Invitado Internacional impartirá unas rigurosas Masterclasses para ahondar en las últimas innovaciones en el abordaje de Dependency-Related Skin Lesions ”
Esta Postgraduate diploma en Dependency-Related Skin Lesions contiene el programa educativo más completo y actualizado del mercado. Sus características más destacadas son:
- El desarrollo de casos prácticos presentados por expertos en Heridas para Enfermería
- Los contenidos gráficos, esquemáticos y eminentemente prácticos con los que está concebido recogen una información científica y práctica sobre aquellas disciplinas indispensables para el ejercicio profesional
- Los ejercicios prácticos donde realizar el proceso de autoevaluación para mejorar el aprendizaje
- Su especial hincapié en metodologías innovadoras
- Las lecciones teóricas, preguntas al experto, foros de discusión de temas controvertidos y trabajos de reflexión individual
- La disponibilidad de acceso a los contenidos desde cualquier dispositivo fijo o portátil con conexión a internet
Profundizarás en el Cuidado de las Heridas en Ambiente Húmedo, lo que facilitará que las heridas cicatricen con una mayor rapidez”
El programa incluye en su cuadro docente a profesionales del sector que vierten en esta capacitación la experiencia de su trabajo, además de reconocidos especialistas de sociedades de referencia y universidades de prestigio.
Su contenido multimedia, elaborado con la última tecnología educativa, permitirá al profesional un aprendizaje situado y contextual, es decir, un entorno simulado que proporcionará una capacitación inmersiva programada para entrenarse ante situaciones reales.
El diseño de este programa se centra en el Aprendizaje Basado en Problemas, mediante el cual el profesional deberá tratar de resolver las distintas situaciones de práctica profesional que se le planteen a lo largo del curso académico. Para ello, contará con la ayuda de un novedoso sistema de vídeo interactivo realizado por reconocidos expertos.
¿Quieres incorporar a tu praxis diaria las estrategias farmacológicas más efectivas para reducir el dolor en el Pie Diabético? Lógralo mediante este programa"
Reforzarás tus conocimientos clave mediante la innovadora metodología Relearning de TECH, logrando una asimilación efectiva de la materia”
Syllabus
Through this program nurses will have a thorough understanding of the pathophysiological processes that lead to the generation of skin lesions. The syllabus will delve into the evaluation of wounds, taking into account their early signs. In this regard, the syllabus will delve into the preparation of the wound bed, which will enable graduates to accurately assess the status of the lesions. The program will also examine the physiology of the skin in relation to Skin Lesions. Therefore, professionals will detect early signs of complications (such as infections or tissue deterioration) and perform rapid interventions.

You will master the most avant-garde techniques for the management of Skin Lesions, including Debridement”
Module 1. Skin Wound Management for Nursing
1.1. Injury Evaluation
1.1.1. Wound Identification and Assessment
1.1.2. Recognition of Early Signs of Wounds
1.1.3. Wound Assessment Tools
1.1.4. Documentation and Monitoring of Wound Progression
1.2. Wound Bed Preparation
1.2.1. Wound Cleaning: Techniques
1.2.2. Enzymatic Debridement
1.2.3. Exudate Management
1.2.4. Stimulation of Granulation: Negative Pressure Therapy, Growth Factors and Hyperbaric Oxygen
1.2.5. Wound Bed Protection
1.3. Wounds According to Typology
1.3.1. Acute Wounds: Cuts, Burns and Fractures
1.3.2. Chronic Wounds: Pressure, Venous and Diabetic Ulcers
1.3.3. Surgical Wounds: Incisions, Excisions, Sutures
1.3.4. Traumatic Wounds: Abrasions, Contusions, Lacerations
1.4. Treatment and Care of Wounds
1.4.1. Advanced Therapies: Negative Pressure Therapy, Hyperbaric Oxygen, Laser Therapy
1.4.2. Pain Management
1.4.3. Wound Follow-Up and Evaluation
1.5. Wound Care in Humid Environment (CAH) and TIME Concept
1.5.1. Principles of CAH Contraindications
1.5.2. TIME: Non-Viable Tissue, Infection or Inflammation, Wound Bed Moisture, Wound Edges
1.5.3. CAH and TIME Implementation: Initial Wound Assessment, Treatment Plan, Follow-Up and Adjustment of the Plan
1.5.4. Scientific Evidence on CAH and TIME: Clinical Practice Guideline
1.6. Wound Physiology Wound Healing Process and Complications
1.6.1. Healing Process: Inflammatory, Proliferative and Remodeling Phase
1.6.2. Factors Affecting Healing: Nutrition, Age and Chronic Diseases
1.6.3. Types of Healing: Healing by First Intention, by Second Intention and by Third Intention
1.6.4. Complications in Healing: Infection, Dehiscence, Keloid
1.6.5. Wound Treatment: Cleaning, Use of Antibiotics, Dressings
1.7. Management of Infection and Wound Complications
1.7.1. Signs of Wound Infection: Redness, Warmth, Pain
1.7.2. Treatment of Infection: Antibiotics, Debridement and Wound Care
1.7.3. Wound Complications: Necrosis, Gangrene, Sepsis
1.7.4. Infection Prevention: Wound Cleansing
1.7.5. Management of Wound Complications
1.8. Management of Wound Care Materials
1.8.1. Selection and Correct Use of Materials
1.8.2. Storage of Materials: Storage Conditions and Inventory Management
1.8.3. Material Handling Safety: Safe Disposal of Used Materials, Accident Prevention
1.9. Comprehensive and Integrated Care Among Different Professionals
1.9.1. Teamwork: Roles and Responsibilities Conflict Resolution
1.9.2. Coordination of Care: Shared Care Plan, Coordination with Other Services, Continuity of Care
1.9.3. Referral to Specialists: Referral and Follow-Up Process
1.9.4. Assessment of Quality of Care: Quality Indicators, Clinical Audits and Continuous Quality Improvement
1.10. Clinical Language in Relation to Wounds
1.10.1. Anatomical, Wound Assessment and Wound Management Terms
1.10.2. Effective Communication: Communication with the Patient and Other Health Care Professionals
1.10.3. Clinical Documentation: Informed Consent
1.10.4. Ethics in Wound Care: Respect for Patient Autonomy, Beneficence and Non-Maleficence, Justice
Module 2. Dependency-Related Skin Lesions
2.1. Dependency-Related Skin Lesions
2.1.1. Dependency-Related Skin Lesions
2.1.1.1. Causes and Risk Factors
2.1.2. Anatomy and Physiology of the Skin in Relation to Dependency-Related Skin Lesions
2.1.2.1. Skin Changes
2.1.3. Impact of Dependency-Related Skin Lesions on the Patient's Quality of Life and on the Health Care System
2.1.3.1. Costs Associated with Treatment
2.1.4. Prevention of Dependence-Related Skin Lesions and Evaluation of the Risk of Dependence
2.1.5. Research, Advances and Resources in the Management of Dependency-Related Skin Lesions in Special Populations
2.1.5.1. Clinical Practice Guidelines
2.2. Assessment of Dependence-Related Skin Lesions
2.2.1. Skin Inspection
2.2.1.1. Identification of Areas of Redness and Signs of Infection
2.2.1.2. Evaluation of Skin Integrity
2.2.2. Measurement of Dependency-Related Skin Lesions
2.2.2.1. Measurement of Size
2.2.2.2. Depth Assessment
2.2.2.3. Tissue Evaluation in the Ulcer Bed
2.2.3. Classification of Dependency-Related Skin Lesions
2.2.3.1. Stages of Dependency-Related Skin Lesions
2.2.3.2. Dependence-Related Skin Lesions, Not Classifiable
2.2.4. Pressure-Related Skin Lesions Due to Medical Devices
2.2.5. Pain Assessment
2.2.5.1. Scales for Assessing Pain
2.2.5.2. Pain Management in Pressure Related Skin Injuries
2.2.5.3. Patient Education in Pain Management
2.2.6. Documentation of Dependency-Related Skin Lesions
2.2.6.1. Photographing and Recording the Evolution
2.2.6.2. Communication with Other Health Professionals
2.3. Treatment of Dependency-Related Skin Lesions
2.3.1. Cleansing of Dependency-Related Skin Lesions
2.3.1.1. Selection of the Cleaning Solution
2.3.1.2. Cleaning Techniques and Frequency
2.3.2. Debridement of Dependency-Related Skin Lesions
2.3.2.1. Types of Debridement
2.3.2.2. Indications and Contraindications
2.3.2.3. Care After Debridement
2.3.3. Selection of Dressings
2.3.3.1. Types, Properties and Change of Dressings
2.3.4. Advanced Therapies
2.3.4.1. Negative Pressure Therapy
2.3.4.2. Hyperbaric Oxygen
2.3.4.3. Biological Therapies
2.3.5. Surgery of Dependency-Related Skin Lesions
2.3.5.1. Indications for Surgery
2.3.5.2. Types of Surgery
2.3.5.3. Postoperative Care
2.4. Management of Exudate from Dependency-Related Skin Lesions
2.4.1. Evaluation of the Exudate
2.4.1.1. Amount of Exudate, Characteristics and Changes in Exudate
2.4.2. Exudate Management
2.4.2.1. Absorbent Dressings, Drains and Dressing Changes
2.4.3. Impact of Exudate on the Perilesional Skin
2.4.3.1. Moisture Dermatitis, Maceration and Protection of the Perilesional Skin
2.4.4. Exudate and Pain
2.4.4.1. Impact of Exudate on Pain
2.4.4.2. Pain Management in Skin Lesions with a lot of Exudate
2.4.4.3. Patient Education
2.4.5. Exudate and Odor
2.4.5.1. Causes of Odor in Skin Lesions
2.4.5.2. Management of Odor: Impact of Odor on the Patient's Quality of Life
2.5. Dependency Related Skin Lesions in Special Populations
2.5.1. Dependence-Related Skin Lesions in Elderly People
2.5.1.1. Risk Factors in People, Prevention and Treatment
2.5.2. Dependency-Related Skin Lesions in Persons with Reduced Mobility
2.5.2.1. Risk Factors, Prevention and Treatment
2.5.3. Dependency-Related Skin Lesions in People with Chronic Diseases
2.5.3.1. Risk Factors, Prevention and Treatment in People with Chronic Diseases
2.5.4. Dependency-Related Skin Lesions in Palliative Care
2.5.4.1. Pain Management, Skin Care and Emotional Support
2.5.5. Research, Advances and Resources on Dependency-Related Skin Lesions in Special Populations
2.5.5.1. Clinical Practice Guidelines
2.6. Nutrition and Dependency-Related Skin Lesions
2.6.1. Nutritional Assessment
2.6.1.1. Body Mass Index
2.6.1.2. Evaluation of Dietary Intake and Nutrient Levels
2.6.2. Nutrients and Pressure Ulcer Healing
2.6.2.1. Proteins, Vitamins and Minerals and Hydration
2.6.3. Nutritional Interventions
2.6.3.1. Nutritional Supplements, Balanced Diet and Dietary Counseling
2.6.4. Nutrition and Comorbidities
2.6.4.1. Diabetes
2.6.4.2. Renal disease
2.6.4.3. Cardiovascular disease
2.6.5. Nutritional Education
2.6.5.1. Importance of Nutrition in the Healing of Pressure Ulcers
2.6.5.2. Foods Beneficial for the Healing of Pressure Ulcers
2.7. Dependency-Related Skin Lesions and Quality of Life
2.7.1. Physical Impact of Dependency-Related Skin Lesions
2.7.1.1. Pain, Mobility Limitations and Sleep Problems
2.7.2. Emotional Impact of Dependency-Related Skin Injuries
2.7.2.1. Stress, Anxiety and Depression Body Image and Self-Esteem
2.7.3. Social Impact of Skin Lesions Related to Dependency
2.7.3.1. Social Isolation, Dependence and Impact on the Family and Caregivers
2.7.4. Assessment of Quality of Life and Pain
2.7.4.1. Quality of Life Assessment Scales
2.7.4.2. Scales for Assessing Pain
2.7.5. Emotional and Social Impact Assessment
2.7.6. Improvement of Quality of Life
2.7.6.1. Pain Management, Psychological Support, and Promotion of Social Participation
2.8. Coordination of Home Care Services in Different Patient Care Settings
2.8.1. Coordination of Home Care Services
2.8.2. Evaluation and Follow-Up by the Home Care Services
2.8.3. Roles and Responsibilities in the Primary Care Team
2.9. Patient and Caregiver Education
2.9.1. Care of Dependency-Related Skin Lesions at Home
2.9.1.1. Ulcer Cleaning, Dressing Changes, Positioning and Mobilization
2.9.1.2. Pain Management at Home
2.9.2. Use of Analgesics
2.9.2.1. Relaxation Techniques and Consultation with the Health Professional in the Event of of Increased Pain
2.9.2.2. Stress Management and Emotional Support for Patients and Caregivers
2.9.3. Research, Advances and Resources in the Improvement of Quality of Life in Patients with Dependency-Related Skin Lesions
2.10. Research and Advances in the Management of Dependency-Related Skin Lesions
2.10.1. Research on Prevention of Dependency-Related Skin Lesions (I)
2.10.1.1. Studies on the Efficacy of Preventive Measures
2.10.1.2. Development of New Pressure-Relieving Devices and Research on Nutrition and Prevention of Pressure Ulcers
2.10.2. Research on Treatment of Dependency-Related Skin Lesions (II)
2.10.2.1. Clinical Trials of New Treatments
2.10.2.2. Research on Pain Management
2.10.2.3. Studies on the Quality of Life of People with Dependence-Related Skin Lesions
2.10.3. Advances in the Care of Dependency-Related Skin Lesions
2.10.3.1. New Dressings and Wound Care Materials
2.10.3.2. Advanced Therapies and Innovations in Education and Training
2.10.4. Participation in Nursing Research
2.10.4.1. Participation in Clinical Trials
2.10.4.2. Nursing Research Training
2.10.4.3. Research Ethics
2.10.5. Research Updates and Advances
2.10.5.1. Scientific Literature, Congresses and Seminars
2.10.5.2. Professional Networks and Interest Groups
Module 3. Diabetic Foot Management for Nursing
3.1. Etiology of the Diabetic Foot
3.1.1. Risk Factors and Underlying Causes
3.1.2. Pathophysiological Mechanisms Involved
3.1.3. Classification According to Neuropathic and Vascular Complications
3.2. Diabetic Foot Assessment
3.2.1. Risk Assessment Methods
3.2.2. Detailed Physical Examination
3.2.3. Use of Complementary Tests
3.3. Prevention of Diabetic Foot
3.3.1. Education on Daily Foot Care
3.3.2. Control of Risk Factors
3.3.3. Secondary Prevention Programs
3.4. Treatment of the Diabetic Foot
3.4.1. Conservative and Surgical Approaches
3.4.2. Use of Advanced Dressings and Innovative Therapies
3.4.3. Multidisciplinary Approach
3.5. Diabetic Foot Care
3.5.1. Ulcer and Lesion Management
3.5.2. Proper Nail and Skin Care
3.5.3. Prevention of Complications
3.6. Pain Management in the Diabetic Foot
3.6.1. Pharmacologic and Non-Pharmacologic Strategies
3.6.2. Treatments Targeting Specific Neuropathies
3.6.3. Pain Self-Management Education
3.7. Nutrition and Diabetic Foot
3.7.1. Assessment of Nutritional Status
3.7.2. Importance of a Balanced Diet
3.7.3. Specialized Dietary Supervision
3.8. Diabetic Foot Care in Geriatric Patients
3.8.1. Frailty-Specific Considerations
3.8.2. Adaptation in Care
3.8.3. Personalized Rehabilitation Programs
3.9. Patient Education on Diabetic Foot Care
3.9.1. Practical Instructions for Self-Care
3.9.2. Recognition of Warning Signs
3.9.3. Importance of Adherence to Treatment
3.10. Advances in the Treatment of the Diabetic Foot
3.10.1. New Technologies in Wound Healing
3.10.2. Research on Regenerative Therapies
3.10.3. Development of Advanced Prostheses and Devices

The interactive summaries of each topic will allow you to consolidate in a more dynamic way the concepts of Skin Lesions with Dependency. Enroll now!”
Postgraduate Diploma in Dependency-Related Skin Lesions
Discover TECH Global University's Postgraduate Diploma in Dependency-Related Skin Lesions, a unique opportunity for nurses who wish to specialize in the advanced management of dermal lesions in dependent patients. This innovative program offers online classes designed to provide fundamental theoretical and practical knowledge, guided by experts in the field of specialized nursing. Today, skin injuries, such as pressure ulcers, represent a significant challenge in the care of dependent patients. These conditions not only affect the patient's quality of life, but also their overall well-being. Therefore, it is crucial that nursing professionals are properly specialized to prevent, identify and effectively treat these injuries. This Postgraduate Diploma program combines the flexibility of online classes with a rigorous focus on the latest clinical practices and protocols. Participants will learn advanced strategies for risk assessment, selection of appropriate treatments and promotion of wound healing, all based on up-to-date scientific evidence.
Study at the best digital university
Do you know why TECH is considered one of the best universities in the world? Because we have a catalog of more than ten thousand academic programs, presence in multiple countries, innovative methodologies, unique academic technology and a highly qualified faculty; that's why you can't miss the opportunity to study with us. Upon completion of this postgraduate diploma, graduates will be prepared to face the specific challenges of skin injuries in long-term care and hospital settings. In addition, they will acquire skills that will not only benefit their patients, but also strengthen their professional development in the skilled nursing field. Don't miss this opportunity to advance your career and become an expert in the management of dependency-related skin injuries - enroll in TECH Postgraduate Diploma in Skin Injuries at TECH Global University of Technology today and make a difference in healthcare!







