University certificate
The world's largest faculty of medicine”
Introduction to the Program
Learn about the new developments in Macula, Retina and Vitreous Pathology and Surgery, and offer a more personalized care to your patients"

This Master's Degree in Macula, Retina and Vitreous Pathology and Surgery deals in depth with all the subspecialties of the retina, delving deeply into other major issues, such as AMD (Age-Related Macular Degeneration). In addition, the specific topics on surgery provide an additional value to this entire educational project, the main objective of which is to offer a high-level qualification to support the need for study of these professionals and increase their professional skills.
Specifically, this program deals exhaustively with diseases such as AMD, which has a wide repercussion in society and in daily life, or tumors, uveitis and infections, for which there is a scarce bibliographic reference, so a high-level qualification such as this will allow our students to obtain an advanced knowledge in this field.
Completion of the Master's Degree will give students the confidence they require for the full development of their profession, covering complex pathologies and surgical processes that they can subsequently develop in their daily clinical-surgical activity. It will also serve as a basis for further consultation in order to solve complex or doubtful cases in their daily work.
The Master's Degree has specialized teaching staff in ocular pathology and surgery, who contribute both their practical experience from their day-to-day work in private practice, as well as their long experience in teaching at a national and international level. In addition, it has the advantage of being a 100% online program, so the student can decide where and when they would like to study. This way, you will be able to flexibly self-manage your study hours.
This Master's Degree is the best option you can find to increase your knowledge in eye disease and give a boost to your professional career"
This Master's Degree in Macula, Retina and Vitreous Pathology and Surgery contains the most complete and up-to-date scientific program on the market. Its most notable features are:
- The development of more than 75 clinical cases presented by experts in ocular pathology and surgery
- The graphic, schematic, and practical contents with which they are created, provide scientific and practical information on the disciplines that are essential for professional practice
- The presentation of practical workshops on procedures and techniques
- An algorithm-based interactive learning system for decision-making in the clinical situations presented throughout the course
- Action protocols and clinical practice guidelines, which cover the most important latest developments in this specialist area
- Theoretical lessons, questions for experts, discussion forums on controversial issues and individual reflection work
- Special emphasis on test-based medicine and research methodologies
- Content that is accessible from any fixed or portable device with an Internet connection
This Master's Degree is the best investment you can make in a qualification to update your knowledge in Macula, Retina and Vitreous Pathology and Surgery"
The teaching staff includes a team of prestigious urologists, who bring their experience to this educational program, as well as renowned specialists from leading scientific societies.
The multimedia content, developed with the latest educational technology, will provide the professional with situated and contextual learning, i.e., a simulated environment that will provide an immersive training experience designed to train for real-life situations.
This program is designed around Problem-Based Learning, whereby the professional must try to solve the different professional practice situations that arise throughout the program. For this reason, you will be assisted by an innovative, interactive video system created by renowned and experienced experts in the field of Macula, Retina and Vitreous Pathology and Surgery with extensive teaching experience.
This 100% online Master's Degree will allow you to study from anywhere in the world. All you need is a computer or mobile device with an internet connection"
Our innovative teaching methodology will allow you to study as if you were dealing with real cases, and therefore increasing your training"
Syllabus
The structure of the syllabus has been designed by a team of professionals who are knowledgeable regarding the implications of medical education in the approach to patients, aware of the relevance of current training and committed to quality teaching through new educational technologies.

This Master's Degree contains the most complete and up-to-date scientific program on the market”
Module 1. Anatomy, Physiology and Exploratory and Functional Tests
1.1. Historical Notes and Classical Exploration in Consultation
1.1.1. History to Understand the Present
1.1.2. The Ophthalmoscope and its Examination Lenses
1.1.3. The Slit Lamp and Its Examination Lenses
1.1.4. Historical Notes of Current Exploration Techniques
1.2. Macula and Retina Anatomy
1.2.1. Compared Anatomy
1.2.2. Macula and Retinal Histology
1.2.3. Vascularization of the Retina and Macula
1.2.4. Innervation of the Retina and Macula
1.3. Vitreous Anatomy and Physiology
1.3.1. Vitreous Embryology
1.3.2. Composition of the Vitreous Gel
1.3.3. Hyaloid Insertions and Adhesions
1.3.4. Aging and Alterations of the Vitreous Gel
1.3.5. The Vitreous in Myopic Patients
1.3.6. The Vitreous in Certain Systemic Diseases
1.3.7. Vitreous as a Trigger for Various Retinal and Macular Pathologies
1.4. Physiology of Vision and Colour Vision
1.4.1. Functional Layers of the Retina
1.4.2. Photoreceptor Physiology
1.4.3. Functional Circuits of the Retina
1.4.4. Optical Route
1.4.5. Physiology of the Visual Cortex
1.4.6. Binocularity
1.4.7. Colour Vision
1.5. Macular Functional Testing
1.5.1. Basis of Macular Functional Testing
1.5.2. Electroretinogram, Electrooculogram and Evoked Potentials
1.5.3. Multifocal Electroretinogram
1.5.4. Microperimetry
1.6. Fundus Photography, Intravenous Fluorescein Angiography and Indocyanine Green Angiography
1.6.1. Analogue and Digital Retinography
1.6.2. Ultra-Widefield Photographic Retinography, Most Important Current Platforms
1.6.3. Properties of Sodium Fluorescein and Its Adverse Effects
1.6.4. Normal AFG Pattern (Angiofluoresceingraphy)
1.6.5. Pathological Angiographic Patterns, Hyperfluorescence, Hypofluorescence and Window Effect
1.6.6. Current Role and Clinical Indications of AFG
1.6.7. Properties of Indocyanine Green and Its Pharmacokinetics
1.6.8. Pathological Angiographic Patterns of Indocyanine Green
1.7. Fundus Autofluorescence
1.7.1. Autofluorescence Detection and Recording
1.7.2. Autofluorescence Detection and Recording
1.7.3. Normal Autofluorescence Patterns
1.7.4. Pathological Autofluorescence Patterns
1.7.5. Autofluorescence in Retinal Diseases
1.8. Ultrasonic Retinal Evaluation
1.8.1. Physical Bases of Ultrasound
1.8.2. Current Platforms and Probes For Ocular Ultrasound Scans
1.8.3. Current Ultrasound Methods and Modes
1.8.4. Ocular Ultrasound Patterns
1.9. Optical Coherence Tomography
1.9.1. Physical Principles of OCT (Optical Coherence Tomography)
1.9.2. Historical Evolution of OCT
1.9.3. Main OCT Platforms and Their Differential Characteristics
1.9.4. Normal OCT Patterns
1.9.5. Comparative Patterns of OCT Monitoring
1.9.6. OCT in Major Macular and Interface Pathologies
1.10. Angiography Using Optical Coherence Tomography
1.10.1. Basis of Angio-OCT
1.10.2. Main Platforms for Performing Angio-OCT
1.10.3. Normal Angio-OCT Patterns
1.10.4. Angio-OCT Analysis and Artefacts
1.10.5. Angio-OCT in the Main Macular Pathologies
1.10.6. Clinical Angio-OCT in Face
1.10.7. The Present and Future of Angio-OCT
Module 2. Vascular Pathology of the Macula and Retina
2.1. Diabetic Retinopathy
2.1.1. Pathophysiology of Diabetic Retinopathy and Metabolic Control
2.1.2. Exploratory Tests in Diabetic Retinopathy
2.1.3. Bio Markers
2.1.4. Diabetic Retinopathy Classification
2.1.5. Non-Proliferative Diabetic Retinopathy
2.1.6. Diabetic Macular Edema
2.1.7. Medical Treatment of Diabetic Macular Edema, Main Treatment Regimens, Main Pharmaceuticals and Supporting Clinical Trials
2.1.8. Pathophysiological Basis for Laser Treatment of NPDR and Diabetic Macular Edema
2.1.9. Current Laser Types and Their Application in NPDR
2.1.10. Laser Treatment Techniques and Patterns
2.1.11. Proliferative Diabetic Retinopathy PDR
2.1.12. Laser Treatment of PDR and Its Combination with Intravitreal Pharmaceuticals
2.1.13. Side Effects of Retinal Panphotocoagulation
2.1.14. Management of Iris Rubeosis
2.2. Branch Retinal Vein and Central Retinal Vein Occlusion
2.2.1. Systemic and Local Risk Factors
2.2.2. Physiopathogenesis
2.2.3. RVO and CRVO Clinic
2.2.4. Functional Tests for the Diagnosis of Venous Obstructions
2.2.5. Medical Treatment of Venous Obstructions. Treatment Guidelines and Current Pharmaceuticals
2.2.6. Current Status of Laser Treatment for Venous Obstructions
2.2.7. Treatment of Neovascularisations Secondary to Venous Obstructions
2.3. Arterial Embolism and Central Retinal Artery Embolism
2.3.1. Pathophysiology
2.3.2. Arterial Branch Occlusion
2.3.3. Central Retinal Artery Occlusion
2.3.4. Ciliary Retinal Artery Occlusion
2.3.5. Arterial Occlusion Associated with Venous Occlusions
2.3.6. Examination of the Patient with Retinal Arterial Obstruction
2.3.7. Medical Treatment of Retinal Artery Blockage
2.4. Retinal Arterial Macroaneurysm
2.4.1. Definition, Pathophysiology and Anatomy
2.4.2. Retinal Macroaneurysm Clinic
2.4.3. Diagnostic Tests for Retinal Macroaneurysm
2.4.4. Differential Diagnosis of Retinal Macroaneurysm
2.4.5. Retinal Macroaneurysm Treatment
2.5. Idiopathic Macular Telangiectasias
2.5.1. Pathophysiology and Classification of Retinal Telangiectasia
2.5.2. Examination of Retinal Telangiectasias
2.5.3. Type 1 Juxtafoveal Telangiectasia
2.5.4. Type 2 Perifoveolar Telangiectasia
2.5.5. Type 3 Occlusive Telangiectasia
2.5.6. Differential Diagnosis of Macular Telangiectasia
2.5.7. Idiopathic Macular Telangiectasia Treatment
2.6. Ocular Ischaemia Syndrome
2.6.1. Definition and Pathophysiology of Ocular Ischaemia Syndrome
2.6.2. OIS Clinic
2.6.3. OIS Screening and Diagnosis
2.6.4. Differential Diagnosis
2.6.5. OIS Treatment
2.7. Arterial Hypertension and Its Retinal Pathology
2.7.1. Pathophysiology of AHT
2.7.2. Malignant Arterial Hypertension
2.7.3. Classification of Hypertensive Retinopathy by Fundoscopic Severity and Its Clinical Signs
2.7.4. Semiology of Hypertensive Retinopathy
2.7.5. AHT Clinic
2.7.6. AHT Treatment and its Retinal Repercussions
2.8. Retinal Pathology Associated with Blood Dyscrasia
2.8.1. Definition and Classification of Retinopathy Associated with Blood Dyscrasias
2.8.2. Screening for Retinopathies Associated with Dyscrasia
2.8.3. Retinal Pathology Associated with Anemic Syndromes, Classification and Ophthalmologic Manifestations
2.8.4. Retinal Pathology Associated with Anemic Syndromes, Classification and Ophthalmologic Manifestations
2.8.5. Retinal Pathology Associated with Blood Hyperviscosity Syndromes. Classification and Ocular Manifestations
2.8.6. Retinal Pathology Associated with Bone Marrow Transplantation and Graft-Versus-Host Disease
2.9. Eales' Disease
2.9.1. Definition and Etiopathogenesis of Eales’ Disease
2.9.2. Clinical symptoms
2.9.3. Exploratory Tests in Eales' Disease
2.9.4. Differential Diagnosis
2.9.5. Medical Treatment, Laser Treatment and Surgical Treatment of Eales' Disease
2.10. Macular and Premacular Hemorrhages
2.10.1. Definition and Etiopathogenesis of Macular and Premacular Hemorrhages
2.10.2. Clinical and Etiological Diagnosis
2.10.3. Exploratory Functional Tests
2.10.4. Treatment of Macular and Premacular Hemorrhages. Laser Treatment, Surgical Treatment
2.10.5. Complications of Macular and Premacular Hemorrhages
Module 3. Diseases of the Pigmentary Epithelium, Bruch's Membrane, Choroid and Pachychoroid
3.1. Radiation Maculopathy
3.1.1. Pathophysiology of Radiation Maculopathy
3.1.2. Histology of Radiation Maculopathy
3.1.3. Examination and Diagnosis of Radiation Maculopathies, Definite Patterns
3.1.4. Clinical Signs of Radiation Maculopathy
3.1.5. Incidence of Radiation Maculopathy
3.1.6. Risk Factors
3.1.7. Treatment of Radiation Maculopathy
3.2. Siderosis and Other Depot Maculopathies
3.2.1. Etiology of Depot Maculopathies
3.2.2. Natural, Clinical History of Depot Maculopathies
3.2.3. Scanning, Angiographic Patterns, Structural OCT and Angio-OCT Changes
3.2.4. Siderosis
3.2.5. Calcosis
3.2.6. Alterations in the ERG of Depot Diseases
3.2.7. Medical Treatment for Depository Diseases
3.2.8. Surgical Treatment of Deposit Diseases
3.3. Light Toxicity
3.3.1. Mechanisms of Photomechanical, Thermal and Photochemical Retinal Damage
3.3.2. Mechanisms of Retinal Damage Due to Chronic Sun Exposure
3.3.3. Mechanisms of Retinal Damage Due to Chronic Sun-Exposure
3.3.4. Electric Arc Welding Injuries
3.3.5. Electric shock injuries
3.3.6. Lightning Retinopathy
3.3.7. Iatrogenic Lesions Associated with Therapeutic Lasers
3.3.8. Macular Lesions Associated with Exposure to Non-Therapeutic Lasers
3.3.9. Treatment of Retinal Diseases Due to Light Exposure
3.4. Drug Toxicity
3.4.1. Pathophysiology of Drug Induced Maculopathy
3.4.2. Examination of the Macula in Drug Toxicity
3.4.3. Functional Diagnostic Tests
3.4.4. Maculopathy Due to Chloroquine and Its Derivatives
3.4.5. Talc, Tamoxifen and Canthaxanthin Maculopathy
3.4.6. Maculopathy Associated with Latanoprost and Other Glaucoma Treatment Drugs, Epinephrine and Nicotinic Acid
3.4.7. Aminoglycoside Maculopathy
3.4.8. Phenothiazine Maculopathy
3.4.9. Deferoxamine Maculopathies
3.4.10. Treatment of Drug Retinopathy
3.5. Subretinal Neovascularisation Associated with Scarring and Other Processes
3.5.1. Etiology of Choroidal Neovascularisation Associated with Scarring
3.5.2. Clinical and Natural History
3.5.3. Scanning, Structural OCT and Angio-OCT, Angiographic Patterns
3.5.4. Idiopathic Causes
3.5.5. Spectrum Inflammatory Diseases, Presumed Ocular Histoplasmosis Syndrome (POHS)
3.5.6. Inflammatory Diseases, Multifocal Choroiditis Syndrome with Panuveitis (MCP)
3.5.7. Inflammatory Diseases, Punctate Inner Choroidopathy (PIC)
3.5.8. Infectious Diseases, Toxoplasmosis
3.5.9. Infectious Diseases, Toxocariasis
3.5.10. Spectrum of Secondary Diseases Due to the Rupture of Bruch's Membrane. Choroidal rupture, Angioid Striae, Iatrogenesis Secondary to Photocoagulation
3.5.11. Spectrum of Diseases Secondary to Alterations in the Pigment Epithelium and Bruch's Membrane. Best's Disease, AMD-like Syndromes
3.5.12. Current Status of the Treatment of Neovascularisation Associated with Inflammatory, Infectious and Other Processes
3.6. Pigment Epithelium Detachment
3.6.1. Definition of Pigment Epithelium Detachment (PED)
3.6.2. Etiology of PED
3.6.3. Types of PED
3.6.4. PED Scanning. Angiographic Patterns, Structural OCT and Angio-OCT
3.6.5. Clinical and Natural History of PED
3.6.6. Intravitreal Treatment for PED-Associated Neovascularisation
3.6.7. Other Treatments for Pigmented Epithelium Detachment
3.7. Angioid Streaks
3.7.1. Definition of Angioid Streaks
3.7.2. Aetiopathogenesis and Pathophysiology
3.7.3. Natural history and Evolution of Angioid Streaks
3.7.4. Diagnosis of Angioid Streaks, Angiographic Patterns, Indocyanine Green Angiography, Autofluorescence, Structural OCT, Angio-OCT
3.7.5. Exploration of Associated Neovascular Complexes
3.7.6. Current Treatments for Angioid Streak Marks and their Associated Neovascular Complexes
3.8. Pachychoroid Diseases
3.8.1. Definition of Pachychoroid Spectrum Disorders
3.8.2. Diagnosis of Pachychoroid Diseases, Common Features
3.8.3. OCT, Angio-OCT Patterns
3.8.4. Pachychoroid Spectrum Diseases, Acute and Chronic Central Serous Choroidopathy. Diagnosis, Characteristics and Up-to-Date Treatment
3.8.5. Pachychoroid Spectrum Diseases, Pachychoroid Pigment Epitheliopathy. Diagnosis, Characteristics and Up-to-Date Treatment
3.8.6. Pachychoroid Neovasculopathy. Diagnosis, Characteristics and Up-to-Date Treatment
3.8.7. Polypoid Choroidal Vasculopathy. Diagnosis, Characteristics and Up-to-Date Treatment
3.8.8. Focal Choroidal Excavation. Diagnosis, Characteristics and Up-to-Date Treatment
3.8.9. Peripapillary Pachychoroid Syndrome. Diagnosis, Characteristics and Up-to-Date Treatment
Module 4. Inflammatory Eye Diseases Involving the Macula, Retina and Vitreous
4.1. Diagnosis and Treatment of Uveitis
4.1.1. Diagnosis of Uveitis
4.1.1.1. Systematic Approach to the Diagnosis of Uveitis
4.1.1.2. Classification of Uveitis
4.1.1.3. Localisation of Uveitis
4.1.1.4. Approach to Patients, the Clinical History as a Diagnostic Asset
4.1.1.5. Detailed Eye Examination. Diagnostic Guidance
4.1.1.6. Most Common Tests Used for the Study of Uveitis
4.1.1.7. Differential Diagnosis Tables
4.1.2. Imaging Tests Used for the Study of Uveitis. Systemic Imaging Tests
4.1.3. Ophthalmological Imaging Tests. Fundus photograph, AFG, ICG, OCT, angio-OCT, BMU, Ultrasound, etc.
4.1.4. General Treatment for Uveitis
4.1.4.1. Corticosteroids
4.1.4.2. Mydriatic and Cycloplegic Agents
4.1.4.3. Nonsteroidal Anti-Inflammatory Drugs
4.1.4.4. Immunosuppressive Treatments
4.1.4.5. New Biological Therapies to Treat Uveitis
4.1.5. Diagnostic Surgery for Uveitis. Retinal Biopsies
4.1.6. Therapeutic Surgery: Cornea, Iris, Cataracts, Glaucoma, Vitreous and Retina. Comprehensive Treatment for Uveitis
4.2. Cystoid Macular Edema
4.2.1. Pathophysiology, Blood-Retinal Barrier Function
4.2.2. Histology of Cystoid, Macular Edema
4.2.3. Mechanisms of Blood-Retinal Barrier Breakage
4.2.4. Exploration of Cystoid Macular Edema. Fluorescein Angiographic Patterns, OCT, Angio-OCT and Clinical in Face
4.2.5. Vitreous Fluorophotometry
4.2.6. Treatment of Post-Surgical Macular Edema
4.3. White Spot Syndromes and Associated Diseases
4.3.1. Birdshot: Chorioretinopathy in Buckshots
4.3.2. Placoid Diseases
4.3.3. Multifocal Choroiditis and Panuveitis, Internal Punctate Choroidopathy Syndrome, and Progressive Subretinal Fibrosis and Uveitis
4.3.4. Multiple Evanescent White Plaques Syndrome. Main Characteristics, Evolution and Differential Diagnosis
4.3.5. Acute Zonal External Retinopathy
4.3.6. Acute Macular Neuroretinopathy
4.4. Acute Multifocal Posterior Placoid Epitheliopathy
4.4.1. Aetiopathogenesis
4.4.2. Clinical Symptoms
4.4.3. Angiographic Scanning Patterns
4.4.4. OCT, Angio-OCT Scanning
4.4.5. Natural History of the Disease
4.4.6. Differential Diagnosis
4.4.7. Treatment
4.5. Serpiginous Choroiditis
4.5.1. Etiopathogenesis of Serpiginous Choroiditis
4.5.2. Clinical and Natural History of the Disease
4.5.3. Techniques for Examining Serpiginous Choroiditis
4.5.4. Angiographic Patterns and Structural OCT
4.5.5. Differential Diagnosis
4.5.6. Treatment
4.6. Vogt-Koyanagi-Harada Syndrome
4.6.1. Introduction and Classification of Vogt-Koyanagi-Harada Syndrome
4.6.2. Macular Damage
4.6.3. Natural History of the Disease
4.6.4. Scanning, Angiographic Patterns, OCT Imaging. Angio-OCT
4.6.5. Differential Diagnosis
4.6.6. Treatment of Associated and Recurrent Neovascular Membranes
4.7. Multifocal Choroiditis
4.7.1. Epidemiology of Multifocal Choroiditis
4.7.2. Etiopathogenesis of Multifocal Choroiditis
4.7.3. Clinical Symptoms
4.7.4. Exploration of Multifocal Choroiditis. Angiographic Patterns, ICG, OCT and angio-OCT
4.7.5. Differential Diagnosis
4.7.6. Natural History of Multifocal Choroiditis
4.7.7. Current Treatment
4.8. Sympathetic Ophthalmia
4.8.1. Epidemiology of Sympathetic Ophthalmia
4.8.2. Pathophysiology of Sympathetic Ophthalmia
4.8.3. Immunopathology of Sympathetic Ophthalmia
4.8.4. Clinical Findings
4.8.5. Scanning, Angiographic Pattern, Structural OCT and Angio-OCT
4.8.6. Differential Diagnosis
4.8.7. Natural History of the Disease, Course and Possible Complications
4.8.8. Treatment, Prevention and Prognosis
4.9. Autoimmune Retinopathies
4.9.1. Epidemiology and Mechanisms of Action
4.9.2. Clinical Manifestations of Autoimmune Retinopathies
4.9.3. Diagnosis, Angiographic Patterns, OCT and Angio-OCT
4.9.4. Differential Diagnosis
4.9.5. Natural History, Evolution and Possible Complications
4.9.6. Local and Systemic Treatments
4.9.7. Prognosis
4.10. Ocular Sarcoidosis
4.10.1. General Considerations in Ocular Sarcoidosis
4.10.2. Natural History and Prognosis of Ocular Sarcoidosis
4.10.3. Ocular Manifestations of Sarcoidosis
4.10.4. Posterior Segment Eye Disease
4.10.5. Ocular Scanning, AFG Patterns, Structural OCT and Angio-OCT
4.10.6. Treatment for Retinal Sarcoidosis
4.11. Intermediate Uveitis
4.11.1. Introduction
4.11.2. Epidemiology and Demography
4.11.3. Clinical Findings, Examination of Intermediate Uveitis
4.11.4. Histopathology of Intermediate Uveitis
4.11.5. Clinical Course and Complications
4.11.6. Treatment for Intermediate Uveitis
4.12. Uveitis Masquerade Syndromes
4.12.1. Malignant Uveitis Masquerade Syndromes
4.12.1.1. Intraocular Central Nervous System Lymphoma
4.12.1.2. Leukemia
4.12.1.3. Malignant Melanoma
4.12.1.4. Retinoblastoma
4.12.1.5. Metastasis
4.12.1.6. Paraneoplastic Syndromes
4.12.2. Uveitis Masquerade Syndromes, Endophthalmitis
4.12.2.1. Chronic Postoperative Endophthalmitis
4.12.2.2. Endogenous Endophthalmitis
4.12.3. Non-Malignant and Non-Infectious Masquerade Syndromes
4.12.3.1. Regmatogenic Retinal Detachment
4.12.3.2. Retinitis Pigmentosa
4.12.3.3. Intraocular Foreign Bodies
4.12.3.4. Pigmentary Dispersion
4.12.3.5. Ocular Ischaemia Syndrome
4.12.3.6. Juvenile Xanthogranuloma
Module 5. Infectious Diseases of the Retina and Vitreous
5.1. General Management of Endophthalmitis
5.1.1. Medical History of the Infection Process
5.1.2. Eye Examination According to the Endophthalmitis Process
5.1.3. Sampling for Cultivation
5.1.4. Gateway and Systemic Treatment
5.1.5. Intravitreal Injection Treatment of the Endophthalmitis Process
5.1.6. Surgical Treatment for Ocular Endophthalmitis
5.2. Eye Infection Due to Human Immunodeficiency Virus (HIV)
5.2.1. Uveitis Due to HIV
5.2.2. Eye Examination in HIV Patients
5.2.3. HIV In Eyes, Chorioretinal Involvement, HIV Retinitis
5.2.4. HIV-Associated Opportunistic Infections Cytomegalovirus Retinitis, Varicella Zoster Virus, Ocular Toxoplasmosis, Pneumocystosis, Tuberculosis, Cryptococcosis, Candidiasis, Other Opportunistic Infections
5.2.5. Uveitis Linked to HIV Drug Treatments
5.2.6. Medical Treatment for Ocular HIV, Systemic Intravitreal and Depot Treatments
5.2.7. Surgical Treatment of HIV Retinitis or Opportunistic Infections
5.3. Mycobacterial Infections
5.3.1. Definition of Mycobacterium Tuberculosis Eye Infection
5.3.2. History and Epidemiology
5.3.3. Clinical presentation
5.3.4. Pathophysiology of Ocular Tuberculosis
5.3.5. Pathophysiology of Ocular Tuberculosis
5.3.6. Tuberculosis Diagnostic Tests, the Tuberculin Skin Test and Other Diagnostic Tests
5.3.7. Ocular Examination, Angiographic Patterns, OCT and Angio-OCT
5.3.8. Treatment of Tuberculosis and Ocular Tuberculosis
5.3.9. Possible Complications and Prognosis of Mycobacterial Infections
5.4. Spirochetal Infections
5.4.1. Definition of Treponema Pallidum Syphilis Infection
5.4.2. History and Epidemiology of Syphilis
5.4.3. Clinical Systemic Presentation
5.4.4. Ocular Clinical Presentation, Treponema Pallidum Uveitis. Anterior and Posterior Uveitis. Clinical Manifestations
5.4.5. Pathophysiology and Pathogenesis
5.4.6. Diagnostic Tests for Treponema Pallidum
5.4.7. Systemic and Ocular Treatment for Syphilis Associated Uveitis
5.4.8. Complications and Prognosis
5.5. Ocular Toxoplasmosis
5.5.1. Definition and Natural History of Toxoplasma Gondii Infection
5.5.2. Pathogenesis, the Toxoplasma Gondii Parasite
5.5.3. Parasite Life Cycle, Transmission
5.5.4. Immunobiology and Epidemiology
5.5.5. Congenital and Acquired Toxoplasmosis. Clinical manifestations
5.5.6. Toxoplasmosis in Immunocompromised Patients
5.5.7. Diagnosis and Examination of Ocular Toxoplasmosis. Fundus Photograph, AFG and ICG. OCT and Angio-OCT
5.5.8. Atypical Forms of Ocular Toxoplasmosis. Angiographic and Retinographic Examination
5.5.9. Differential Diagnosis
5.5.10. Diagnostic Tests for Toxoplasma Gondii
5.5.11. Surgical Treatment for Ocular Endophthalmitis
5.5.12. Surgical Treatment of Ocular Toxoplasmosis
5.5.13. Prevention, Prognosis and Conclusions
5.6. Toxocariasis Eye Infection
5.6.1. Definition of Infection Caused by Toxocara Canis or Toxocara Cati
5.6.2. Etiology, the Micro-Organism, Its Life Cycle and Human Infection
5.6.3. Systemic and Ocular Clinical Manifestations
5.6.4. Natural History of Toxocariasis
5.6.5. Immunopathology
5.6.6. Diagnostics, Diagnostic and Serological tests
5.6.7. Ocular Complications of Toxocariasis
5.6.8. Differential Diagnosis of Toxocariasis
5.6.9. Medical and Surgical Treatment of Toxocariasis
5.6.10. Prognosis and Conclusions on Ocular Toxocariasis
5.7. Ocular Ascariasis
5.7.1. Definition of Ascaris Lumbricoides Nematode Infection
5.7.2. Natural History and Epidemiology
5.7.3. Systemic Clinical Features
5.7.4. Ocular Symptoms of Ascariasis
5.7.5. Immunology, Pathology and Pathogenesis, the Life Cycle
5.7.6. Systemic Diagnosis and Ocular Diagnosis. Basic Functional and Imaging Tests
5.7.7. Systemic Treatment and Eye Treatment
5.7.8. Possible Complications and Conclusions
5.8. Ocular Onchocerciasis
5.8.1. Definition of Onchocerca Volvulus Infection
5.8.2. Natural History, Epidemiology, Geographical Distribution
5.8.3. Demographic Factors, Ecology and Biology of Onchocerciasis
5.8.4. Systemic Clinical Manifestations of Onchocerciasis
5.8.5. Ophthalmological Symptoms of Onchocerciasis, Anterior Pole and Posterior Segment Involvement
5.8.6. Etiology, Transmission, Life Cycle of Onchocerca Volvulus
5.8.7. Pathogenesis and Pathology
5.8.8. Clinical and Laboratory Diagnostics
5.8.9. Differential Diagnosis
5.8.10. Systemic and Ocular Treatment of Onchocerciasis
5.8.11. Natural History and Prognosis
5.9. Ocular Loiasis
5.9.1. Definition of Loa-Loa Filaria Infection
5.9.2. History, Epidemiology, Morphology
5.9.3. Systemic Clinical and Ocular Manifestations Anterior Pole and Posterior Pole
5.9.4. Systemic and Ocular Diagnosis
5.9.5. Systemic and Ocular Treatment
5.9.6. Prevention and Chemoprophylaxis
5.10. Ocular Cysticercosis
5.10.1. Definition of Cysticercus Cellulose Infection
5.10.2. History and Epidemiology
5.10.3. Systemic and Ocular Clinical Features
5.10.4. Pathogenesis and Pathology
5.10.5. Systemic and Ocular Diagnosis, Imaging Tests. Ultrasound
5.10.6. Differential Diagnosis
5.10.7. Treatment According to the Location of the Larvae
5.10.8. Complications and Prognosis
5.11. Ocular Borreliosis
5.11.1. Definition of Lyme Disease Due to Borrelia Burgdorferi Infection
5.11.2. History and Epidemiology
5.11.3. Systemic Clinical Symptoms According to Staging
5.11.4. Ocular Clinical Manifestations, Early Disease, Disseminated and Persistent Disease
5.11.5. Pathogenesis
5.11.6. Systemic Diagnosis and Ocular Diagnosis
5.11.7. Systemic and Ocular Treatment
5.11.8. Prognosis, Possible Complications
5.12. Bartonella Eye Infection
5.12.1. Definition of Bartonella Infections
5.12.2. History and Epidemiology
5.12.3. Systemic and Ocular Clinical Features, Retinal and Vitreous Damage
5.12.4. Pathogenesis and Immunology
5.12.5. Systemic Diagnosis and Ocular Diagnosis
5.12.6. Systemic and Ocular Treatment for Bartonellosis
5.12.7. Differential Diagnosis
5.12.8. Prognosis and Conclusions
5.13. Leptospirosis and Eye Infection
5.13.1. Definition of Leptospira Interorgan Infection
5.13.2. Epidemiology
5.13.3. Clinical Features of Non-Ocular Disease
5.13.4. Clinical Signs of Leptospira Eye Disease
5.13.5. Pathogenesis
5.13.6. Laboratory Diagnostics and Ocular Diagnostics
5.13.7. Differential Diagnosis
5.13.8. Systemic and Ocular Treatment of Leptospira Infection
5.13.9. Prognosis and Conclusions
5.14. Ocular Brucellosis
5.14.1. Definition of Brucellosis Infection
5.14.2. History, Etiology, Epidemiology
5.14.3. Molecular Genetics, Pathology and Immunology
5.14.4. Systemic Clinical Features, Subclinical, Acute, Subacute and Chronic Disease
5.14.5. Ocular Manifestations
5.14.6. Systemic and Ocular Diagnosis
5.14.7. Systemic and Ocular Treatment for Bartonellosis
5.14.8. Prognosis, Prevention and Conclusions
5.15. Ocular Whipple's Disease
5.15.1. Definition Signs of Leptospira Eye Disease
5.15.2. History, Epidemiology, Etiology, Pathology and Immunology
5.15.3. Extraocular Clinical Features
5.15.4. Ocular Clinical Features, Uveitis, Neurophthalmology
5.15.5. Systemic and Ocular Diagnosis
5.15.6. Differential Diagnosis
5.15.7. Systemic and Ocular Medical Treatment. Surgical Management
5.15.8. Prognosis and Conclusions
5.16. Rickettsial Eye Disease
5.16.1. Definition, Microbiological Characteristics and Classification of Rickettsioses
5.16.2. History Epidemiology. Pathophysiology. Immunology Pathology and Pathogenesis
5.16.3. Clinical Characteristics. Systemic and Ocular Involvement
5.16.4. Systemic, Laboratory and Ocular Diagnosis
5.16.5. Systemic and Ocular Treatment
5.16.6. Prognosis, Complications and Conclusions on Ocular Rickettsiosis
5.17. Eye Leprosy
5.17.1. Definition of Ocular Hansen's Disease Caused by Mycobacterium Leprae
5.17.2. History and Epidemiology
5.17.3. Systemic and Ocular Clinical Features
5.17.4. Posterior Segment Ocular Complications. Ocular Changes During Acute Leprosy Reactions
5.17.5. Ocular Histopathology
5.17.6. Pathogenesis and Immunology
5.17.7. Systemic and Ocular Diagnosis
5.17.8. Differential Diagnosis
5.17.9. Treatment of Systemic Disease and Eye Disease
5.17.10. Management of Ocular Complications
5.18. Eye Infections Due to the Herpes Virus
5.18.1. Virology, Herpes Simplex Virus and Varicella-Zoster Virus
5.18.1.1. Clinical Features, Acute Retinal Necrosis and Other Retinopathies
5.18.1.2. Diagnostics, Functional and Imaging tests, AFG, OCT and Angio-OCT
5.18.1.3. Differential Diagnosis of Acute Retinal Necrosis
5.18.1.4. Treatment of Acute Retinal Necrosis, Antiviral Agents. Treatment of Associated Retinal Detachment
5.18.2. Eye Infection Due to Epstein-Barr Virus
5.18.3. Cytomegalovirus Eye Infections
5.18.3.1. Ocular Clinical Features
5.18.3.2. Systemic and Ocular Treatment
5.18.4.3. Complications, Prognosis and Conclusions of Cytomegalovirus Infection
5.19. Rubella Eye Disease. Measles Disease
5.19.1. Definition of Measles or Rubella Disease
5.19.2. History
5.19.3. Congenital Rubella
5.19.4. Acquired Rubella
5.19.5. Subacute Sclerosis Subacute Panencephalitis
5.19.6. Treatment for Ocular Rubella
5.19.7. Prognosis and Conclusions
5.20. Presumptive Ocular Histoplasmosis Syndrome
5.20.1. Definition
5.20.2. History, Mycology and Epidemiology
5.20.3. Clinical Features, Disseminated choroiditis, Maculopathy
5.20.4. Pathogenesis, Pathophysiology, Immunology
5.20.5. Laboratory Diagnostics and Ocular Diagnostics, Imaging Tests
5.20.6. Differential Diagnosis
5.20.7. Laser Treatment, Corticosteroid Treatment and Other Currently Proposed Treatments
5.20.8. Submacular and Subretinal Surgery. Complications
5.20.9. Prognosis and Conclusions
5.21. Ocular Candidiasis
5.21.1. Definition of Candida Eye Infection
5.21.2. History and Epidemiology
5.21.3. Clinical Features, Endogenous and Exogenous Candida Endophthalmitis
5.21.4. Complications, Pathogenesis, Histopathology and Immunology
5.21.5. Diagnosis. Vitreous and Anterior Chamber Aspiration
5.21.6. Differential Diagnosis
5.21.7. Systemic and Medical Treatment. The Role of Vitrectomy
5.21.8. Prognosis and Conclusions
5.22. Ocular Amebiasis
5.22.1. Definition of Acanthamoeba and Naegleria Eye Infection
5.22.2. History and Microbiology
5.22.3. Epidemiology, Pathophysiology
5.22.4. Clinical Ocular Disease, Anterior Pole, Uveitis and Late Complications
5.22.5. Diagnostics, Confocal Microscopy, Laboratory Diagnostics
5.22.6. Histology, Cultures
5.22.7. Differential Diagnosis
5.22.8. Medical Treatment, the Value of Vitrectomy and Cryotherapy
5.22.9. Prevention, Prognosis and Conclusions
Module 6. Hereditary Retinal Dystrophies and Pediatric Retinal Pathology
6.1. Hereditary Retinal dystrophies
6.1.1. Clinical Diagnosis. In-clinic Tests and Campimetry
6.1.2. Imaging Tests, OCT and Angio-OCT, Autofluorescence (AF), Fluorescein Angiography and Indocyanine Green
6.1.3. Electrophysiological Study
6.1.3.1. Generalised Photoreceptor Dystrophies
6.1.3.2. Macular Dystrophies
6.1.3.3. Generalised Choroidal Dystrophies
6.1.3.4. Hereditary Vitreoretinopathies
6.1.3.5. Albinism
6.1.4. HRD in the Pediatric Age Group, Main Signs and Symptoms
6.1.5. Genetic Basis of HRD
6.1.6. Clinical Classification of HRD
6.1.6.1. Introduction
6.1.6.2. HRD and Non-Syndromic Vitreoretinal
6.1.6.2.1. Rod Diseases
6.1.6.2.1.1. Stationary: Stationary Night Blindness. With Normal and Abnormal Fundus (Fundus Albipunctatus and Oguchi Disease)
6.1.6.2.1.2. Progressives: Retinitis Pigmentosa (RP) or Cone-Rod Dystrophies (CRD)
6.1.6.2.2. Cone Diseases
6.1.6.2.2.1. Stationary or Cone Dysfunctions: Congenital Achromatopsia
6.1.6.2.2.2. Cone and Cone-Rod Dystrophies (CRD)
6.1.6.2.3. Macular Dystrophies
6.1.6.2.3.1. Stargardt/Fundus Flavimaculatus
6.1.6.2.3.2. Best's Disease
6.1.6.2.3.3. Central Areolar Choroidal Dystrophy (CACD)
6.1.6.2.3.4. X-linked Juvenile Retinoschisis
6.1.6.2.3.5. Other Macular Dystrophies
6.1.6.2.4. Widespread Photoreceptor Diseases
6.1.6.2.4.1. Choroideremia
6.1.6.2.4.2. Atrophy Gyrate
6.1.6.2.5. Exudative and Non-Exudative Vitreoretinopathies
6.1.6.3. Syndromic HRD
6.1.6.3.1. Usher Syndrome
6.1.6.3.2. Bardet Biedl Syndrome
6.1.6.3.3. Senior Loken Syndrome
6.1.6.3.4. Refsum’s Disease
6.1.6.3.5. Joubert´s Disease
6.1.6.3.6. Alagille’s Disease
6.1.6.3.7. Alström's Syndrome
6.1.6.3.8. Neuronal Ceroid Lipofuscinosis
6.1.6.3.9. Primary Ciliary Dyskinesia (PCD)
6.1.6.3.10. Stickler’s Disease
6.1.7. HRD Treatment
6.1.7.1. Gene Therapy A New Future for Treating Diseases with Genetic Alterations. Luxturna
6.1.7.2. Neurotrophic Growth Factor Therapies
6.1.7.3. Cell Therapy
6.1.7.4. Artificial Vision
6.1.7.5. Other Treatments
6.2. Retinopathy of Prematurity
6.2.1. Introduction and Historical Recollection
6.2.2. ROP Classification
6.2.3. Disease Context and Risk Factors
6.2.4. Diagnosis, Screening and Follow-up Guidelines in ROP
6.2.5. ROP Treatment Criteria
6.2.6. Using Anti-Vascular Endothelium Grown Factor
6.2.7. Use of Laser Treatment Today
6.2.8. Treatment by Scleral Surgery and/or Vitrectomy in Advanced Stages
6.2.9. Sequelae and Complications Arising from ROP
6.2.10. Criteria for Discharge and Subsequent Follow-up
6.2.11. Accountability, Documentation and Communication
6.2.12. Future of Screening and New Treatment Options
6.2.13. Medical-Legal Considerations
6.3. Albinism
6.3.1. Introduction and Definitions
6.3.2. Examination and Clinical Findings
6.3.3. Natural History
6.3.4. Treatment and Management of Albino Patients
6.4. X-linked Congenital Retinoschisis
6.4.1. Definition, Genetical Study and Family Tree
6.4.2. Examination and Clinical Findings
6.4.3. Electrophysiological Tests
6.4.4. Classification
6.4.5. Natural History and Genetic Counselling
6.4.6. Treatment Guidelines According to Staging
6.5. Best's Disease
6.5.1. Definition, Genetic Study
6.5.2. Diagnosis, Clinical Findings, Imaging Tests
6.5.3. Functional Testing, Microperimetry and Electrophysiological Testing
6.5.4. Natural History, Clinical Course
6.5.6. Current and Future Treatments for Best's Disease
6.6. Stargardt's Disease, Fundus Flavimaculatus
6.6.1. Definition and Genetic Study
6.6.2. Clinical Findings in Consultation, Imaging Tests
6.6.3. Electrophysiological Tests
6.6.4. Evolutionary History and Genetic Counselling
6.6.5. Current Treatments
6.7. Familial Exudative Vitreoretinopathy. (RVEF)
6.7.1. Definition, Genetic Study
6.7.2. RVEF Clinical Findings
6.7.3. Imaging Tests, OCT, Angio-OCT. AFG
6.7.4. Natural History and Progression of the Disease, Staging
6.7.5. RVEF Laser Treatment
6.7.6. Treatment with RVEF Vitrectomy
6.7.7. Treating Complications
6.8. Persistent Foetal Vasculature Syndrome. (PFVS)
6.8.1. Definition and Evolution of Disease Nomenclature
6.8.2. Ultrasound Examination, Imaging Tests
6.8.3. Clinical Findings in Consultation
6.8.4. Treatment Guidelines and Staging
6.8.5. Surgical Treatment of PFVS. Vitrectomy
6.8.6. Natural and Evolutionary History of the Disease
6.8.7. Visual Rehabilitation
6.9. Coat’s Disease
6.9.1. Definition of Coat’s Disease Evolving Forms
6.9.2. Clinical Findings in Consultation
6.9.3. Imaging Studies, Retinography, AFG, OCT Angio-OCT
Evolving Forms
6.9.4. Ocular Ultrasound in Coat’s Disease
6.9.5. Treatment Spectrum According to the Developmental Form. Natural History
6.9.6. Laser Treatment and Cryotherapy
6.9.7. Treatment by Vitrectomy in Advanced Forms
6.9.8. Visual Rehabilitation
6.10. Norrie's Disease
6.10.1. Definition, Genetic Study
6.10.2. Clinical Findings in Consultation
6.10.3. Treatment Guidelines and Genetic Counselling Treatment Guidelines and Current Pharmaceuticals
6.10.4. Natural and Evolutionary History of Norrie’s Disease
6.11. Incontinentia Pigmenti
6.11.1. Definition and Genetic Study
6.11.2. Clinical Findings and Functional Tests
6.11.3. Natural and Evolutionary History of the Disease
6.11.4. Current Therapeutic Possibilities, Visual Aids
6.12. Choroidal Neovascularisation in the Pediatric Age Group
6.12.1. Clinical Findings in Consultation
6.12.2. Basic Functional and Imaging Tests
6.12.3. Differential Diagnosis
6.12.4. Treatment Guidelines and Their Possibilities According to Age
6.13. Retinal Detachment in the Pediatric Age and Detachment Associated with Ocular Coloboma
6.13.1. General Considerations
6.13.2. Anatomy and Surgical Adaptation to Retinal Detachment Morphology
6.13.3. Peculiarities of Surgery in the Pediatric Age Group, Specialized Surgical Instruments and Equipment for Young Children
6.13.4. Scleral Surgery in the Pediatric Age Group
6.13.5. Vitrectomy in the Pediatric Age Group
6.13.6. Post-Surgical Medical and Postural Treatment in Infancy
6.13.7. Visual Rehabilitation
6.14. Stickler’s Syndromes
6.14.1. Definition and Classification of Stickler Syndromes
6.14.2. Clinical Findings and Imaging Tests
6.14.3. Systemic and Ocular Treatment for the Disease
6.14.4. Current Treatment for Stickler Syndrome
6.14.5. Natural and Evolutionary History of the Disease
6.15. Marfan Syndrome
6.15.1. Definition and Genetic Study of the Disease
6.15.2. Systemic Spectrum of the Disease
6.15.3. Ocular Involvement in Marfan Disease
6.15.4. Ocular Clinical Findings
6.15.5. Applicable Treatments to Marfan Syndrome
6.15.6. Retinal Detachment in Marfan Syndrome
6.15.7. Natural and Evolutionary History of the Disease
Module 7. Age-Related Macular Degeneration (AMD)
7.1. Epidemiology of AMD
7.1.1. Introduction
7.1.2. International Classification Systems, Classification History
7.1.3. Incidence
7.1.4. Prevalence
7.1.5. Etiopathogenesis
7.1.6. Risk Factors
7.2. Genetics of Age-Related Macular Degeneration
7.2.1. Introduction
7.2.2. Genetic Studies Associated with AMD
7.2.3. Complement H Factors and Loci Involved in AMD
7.2.4. Other Factors Implicated in AMD
7.3. Histopathology of AMD
7.3.1. Ocular Ageing, Changes in the Various Retinal Structures
7.3.2. Histological Changes in the Developmental Form of AMD
7.3.3. Changes in the Various Retinal Structures and Pigmented Epithelium
7.3.4. Drusen
7.3.5. Incipient Atrophy
7.3.6. Geographical Atrophy
7.3.7. Neovascular Age-Related Macular Degeneration
7.4. Clinical and Angiographic Findings in AMD. FAG and ICG
7.4.1. Clinical Signs and Symptoms of AMD
7.4.2. Drusen
7.4.3. Pigment Changes
7.4.4. Geographical Atrophy
7.4.5. Pigment Epithelium Detachment PED
7.4.6. Subretinal Neovascular Complexes
7.4.7. Disciform Shapes
7.4.8. Angiographic Study with Fluorescein and Indocyanine Green. Current Applications of the Technique
7.5. Optical Coherence Tomography and Angio-OCT in Age-related Macular Degeneration
7.5.1. OCT and Angio-OCT as a Basis for Disease Monitoring
7.5.2. Initial Information on the Technology
7.5.3. OCT in Early Stages of the Disease
7.5.4. OCT and Angio-OCT, in Geographic Atrophic Forms of the Disease
7.5.5. OCT and Angio-OCT, in Quiescent Forms
7.5.6. Exudative AMD and its Examination with OCT and Angio-OCT
7.5.7. OCT in Retinal Pigment Epithelial Detachments
7.5.8. OCT and Angio-OCT, in Other Forms of Presentation of AMD
7.5.9. Importance of OCT in Clinical Trials for Drug Development and Drug Comparisons in AMD
7.5.10. Prognostic Factors of OCT and Angio-OCT in AMD. Biomarkers
7.6. Updated Classification of AMD and its Correspondence with Previous Classifications
7.6.1. Type 1 Neovascularisation
7.6.2. Type 2 Neovascularisation
7.6.3. Type 3 Neovascularisation
7.6.4. Type 1 Aneurysmal Dilatations or Polypoidal Choroidal Vasculopathy
7.7. Treatment of Atrophic and Degenerative Forms of AMD
7.7.1. Introduction
7.7.2. Diet and Nutritional Supplements in AMD Prevention
7.7.3. The Role of Antioxidants in the Evolutionary Control of the Disease
7.7.4. What Would Be the Ideal Marketing Combination?
7.7.5. Role of Sun-Protection in AMD
7.8. Disused Treatments for Neovascular Forms of AMD
7.8.1. Laser Treatment in AMD, Historical Implications
7.8.2. Types of Lasers for Retinal Treatment
7.8.3. Mechanism of Action
7.8.4. Historical Results and Recurrence Rate
7.8.5. Indications and Instructions for Use
7.8.6. Complications
7.8.7. Transpupillary Thermotherapy as a Treatment for AMD
7.8.8. Epiretinal Brachytherapy for the Treatment of AMD
7.9. Current Treatments for Neovascular Forms of AMD
7.9.1. Photodynamic Therapy for Some Cases of AMD. Historical Recollections of Their Use
7.9.2. Macugen
7.9.3. Ranibizumab
7.9.4. Bevacizumab
7.9.5. Aflibercept
7.9.6. Brolucizumab
7.9.7. Role of Corticosteroids for some types of AMD
7.10. New Treatments for Exudative AMD
7.11. Combined Therapies for AMD
7.12. Systemic Impact of Intravitreal Drugs for AMD
7.12.1. Cardiovascular Risk Factors in AMD
7.12.2. Half-life of Different Intravitreal Drugs in AMD
7.12.3. Adverse Effects in Major Studies of Intravitreal Drugs
Module 8. Tumour Pathology of the Retina, Choroid and Vitreous
8.1. Retinoblastoma
8.1.1. Definition
8.1.2. Genetics of Retinoblastoma
8.1.3. Retinoblastoma Disease. Histopathology
8.1.4. Presentation, Diagnosis and Exploration, Imaging Techniques for Children
8.1.5. Differential Diagnosis
8.1.6. Classification
8.1.7. Retinoblastoma Treatment
8.1.7.1. Chemotherapy/Chemoreduction/Intra-Arterials
8.1.7.2. Thermotherapy
8.1.7.3. Photocoagulation
8.1.7.4. Cryotherapy
8.1.7.5. Brachytherapy
8.1.7.6. External Radiotherapy
8.1.7.7. Enucleation
8.1.7.8. Extraocular Retinoblastoma
8.1.8. Regression Patterns
8.1.9. Visual Rehabilitation and Prognosis
8.2. Cavernous Hemangioma and Racemose Hemangioma
8.2.1. Definition
8.2.2. Clinical Symptoms
8.2.3. Prognosis
8.2.4. Diagnosis and Histology
8.2.5. Treatment
8.3. Retinal Capillary Hemangioblastoma and VonHippel-Lindau Disease
8.3.1. Definition
8.3.2. Clinical Symptoms
8.3.3. Diagnostic Techniques
8.3.4. Differential Diagnosis
8.3.5. Treatment
8.3.6. Complications
8.3.7. Results
8.4. Tuberous Sclerosis and Its Ophthalmological Pathology
8.4.1. Definition
8.4.2. Systemic Manifestations
8.4.3. Ocular Manifestations
8.4.4. Genetic Studies
8.5. Phacomatosis
8.5.1. Definition
8.5.2. Definition of Hamartoma, Choristoma
8.5.3. Neurofibromatosis (Von Recklinghausen Syndrome)
8.5.4. Encephalofacial Hemangiomatosis (Sturge-Weber Syndrome)
8.5.5. Hemangiomatosis Racemose (Wyburn-Mason Syndrome)
8.5.6. Retinal Cavernous Hemangiomatosis
8.5.7. Phacomatosis Vascular Pigment
8.5.8. Oculo-dermal Melanocytosis
8.5.9. Other Phacomatoses
8.6. Retinal Metastases
8.6.1. Definition
8.6.2. Systemic Study Following the Finding of a Possible Metastasis
8.6.3. Eye Study
8.6.4. Treatment
8.7. Distant Effects of Cancer in the Retina. Paraneoplastic Syndromes
8.7.1. Definition
8.7.2. Cancer-Associated Retinopathy Syndrome
8.7.3. MAR Cutaneous Melanoma-Associated Retinopathy Syndrome
8.7.4. Treatment of Paraneoplastic Retinopathies
8.7.5. Bilateral Diffuse Uveal Melanocytic Diffuse Melanocytic Proliferation
8.8. Melanocytoma of the Optic Nerve
8.8.1. Definition
8.8.2. Clinical Findings of Optic Nerve Melanocytoma
8.8.3. Pathology and Pathogenesis
8.8.4. Exploration and Diagnostic Approach
8.8.5. Treatment
8.9. Congenital Hypertrophy of Pigmented Epithelium
8.9.1. Definition
8.9.2. Epidemiology and Demography
8.9.3. Clinical Findings and Classification
8.9.4. Differential Diagnosis
8.10. Combined Pigment Epithelium and Retinal Hamartoma
8.10.1. Definition
8.10.2. Epidemiology
8.10.3. Clinical Manifestations
8.10.4. Examination in Consultation, Diagnosis
8.10.5. Differential Diagnosis
8.10.6. Clinical Course
8.10.7. Etiology and Pathology
8.10.8. Histopathology
8.10.9. Treatment
8.11. Choroidal Nevus
8.11.1. Definition and Prevalence
8.11.2. Choroidal Nevus and Systemic Disease
8.11.3. Histopathology
8.11.4. Clinical Findings in Consultation
8.11.5. Differential Diagnosis
8.11.6. Natural History of Choroidal Nevus
8.11.7. Observation and Monitoring of Choroidal Nevi
8.12. Choroidal Melanoma
8.12.1. Epidemiology
8.12.2. Prognosis and Natural History of Uveal Melanoma
8.12.3. Molecular Genetics of Choroidal Melanoma
8.12.4. Pathology of Choroidal Melanoma
8.12.5. Management and Treatment of Choroidal Melanoma
8.12.5.1. Enucleation
8.12.5.2. Brachytherapy for Choroidal Melanoma
8.12.5.3. Endoresection by Vitrectomy of Choroidal Melanoma
8.12.5.4. Abexternal Resection of Choroidal Melanoma
8.12.6.5. Laser in Choroid Treatment, Transpupillary Thermotherapy
Abexternal Resection of Choroidal Melanoma
8.12.7.6. Photodynamic Therapy for the Treatment of Uveal Melanoma
8.13. Choroidal Metastases
8.13.1. Definition
8.13.2. Incidence and Epidemiology
8.13.3. Clinical Findings and Exploration
8.13.4. Differential Diagnosis
8.13.5. Pathology and Pathogenesis
8.13.6. Treatment
8.13.7. Prognosis
8.14. Choroidal Osteoma
8.14.1. Definition and Epidemiology
8.14.2. Clinical Findings and Exploration
8.14.3. Differential Diagnosis
8.14.4. Pathology and Pathogenesis
8.14.5. Diagnostic Approach
8.14.6. Treatment
8.14.7. Prognosis
8.15. Circumscribed Choroidal Hemangioma
8.15.1. Definition
8.15.2. Clinical Symptoms
8.15.3. Diagnostic Methods, AFG, ICG, Ocular Ultrasound, CT and MRI, OCT
8.15.4. Treatment
8.16. Diffuse Choroidal Hemangioma
8.16.1. Definition
8.16.2. Clinical Symptoms
8.16.3. Diffuse Choroidal Hemangioma
8.16.4. Treatment
8.17. Uveal Tumours
8.17.1. Ciliary Body Epithelial Tumours. Acquired and Congenital
8.17.2. Leukemias and Lymphomas. Primary Vitreous Retinal Lymphoma
Module 9. Introduction to Retinal Surgery, Vitrectomy Arising from Complications of Anterior Segment Surgery, Surgery of the Diabetic Patient, Endophthalmitis and Virus Retinitis
9.1. Instruments, Materials and Therapeutic Alternatives
9.1.1. Methods to Induce Chorioretinal Adhesion
9.1.2. Scleral Surgery Equipment
9.1.3. Gases for Intraocular Use
9.1.4. Silicone Oils
9.1.5. Perfluorocarbons
9.1.6. Cryotherapy
9.1.7. The Vitrectomy, Surgical Principles and Techniques
9.1.8. Different Sizes and Systems of Vitrectomy Probes
9.1.9. Endocular Light Sources and Diversity of Light Terminals
9.1.10. Endovascular Lasers
9.1.11. Accessory Instruments
9.1.12. Visualisation Systems in Vitrectomy. Surgical Lenses. Wide Field
9.1.13. Microscope Systems, 3D Microscopes
9.2. Advanced Vitrectomy Techniques
9.2.1. Simple Vitrectomy. Location of Pars Plana
9.2.2. Pars Plana Lensectomy
9.2.3. Endocyclophotocoagulation
9.2.4. Endolaser Techniques
9.2.5. Liquid Air Exchange Techniques. Gas Injection Techniques
9.2.6. Liquid Perfluorocarbon Injection Techniques
9.2.7. Techniques for the Use and Injection of Silicone Oils
9.2.8. Control of Intraocular Hemorrhage During Surgery
9.2.9. Pupil Management, Pupillary Opening, for Visualisation in Vitrectomy
9.2.10. Handling for Removal of Air or Subretinal Substances
9.3. Surgical Techniques for the Management of Complications Arising from Cataract Surgery
9.3.1. Anterior Vitrectomy
9.3.2. Vitrectomy of Dislocated Crystalline Lens to Vitreous or Crystalline Debris in Vitreous
9.3.3. Surgical Techniques to Manage Dislocated Vitreous Lenses
9.3.4. Techniques for Secondary Lens Implantation in the Absence of a Capsular Bag. Current Lens Models
9.3.5. Techniques for the Treatment of Vitreous Incarcerations
9.4. Glaucoma-Related Vitrectomy Techniques
9.4.1. Filter Surgery and Vitrectomy
9.4.2. Lensectomy and Vitrectomy in the Presence of Leakage Blebs
9.4.3. Techniques for the Management of Pupillary and Angular Blockade
9.4.4. Techniques for Vitreous Chamber Valve Device Implantation
9.5. Diagnostic Biopsy
9.5.1. Biopsy Techniques for the Anterior Segment
9.5.2. Techniques for Vitreous Biopsy and Collection of Material for Analysis
9.5.3. Retinal Biopsy Techniques
9.5.4. Uveal Biopsy Techniques
9.6. Vitrectomy in Diabetes Mellitus
9.6.1. Indications for Surgery in DM
9.6.2. Vitrectomy of Simple Hemorrhage
9.6.3. Vitrectomy for Diabetic Tractional Detachment
9.6.4. Vitrectomy for Progressive Fibrovascular Proliferation
9.6.5. Vitrectomy for Dense Macular Hemorrhages
9.6.6. Vitrectomy in Diabetic Rhegmatogenous Detachment
9.6.7. Use of Silicone in the Diabetic Patient
9.7. Vitrectomy for Endophthalmitis
9.7.1. Pharmacological Management of Endophthalmitis
9.7.2. Sampling for Microbiology
9.7.3. Vitrectomy of the Patient with Endophthalmitis
9.8. Vitrectomy for Retinitis Due to Viruses
9.8.1. Vitrectomy in Herpes Simplex Retinitis
9.8.2. Vitrectomy in Cytomegalovirus Retinitis
9.8.3. Other Herpetic Retinitis
9.8.4. Vitrectomy in Acute Retinal Necrosis
9.8.5. Intravitreal Antiviral Agents
9.9. Intravitreal Pharmaceuticals
9.9.1. Slow-Release Implants
9.9.2. Intravitreal Agents, Miscellaneous
Module 10. Comprehensive Treatment for Retinal Detachment
10.1. Retinal Detachment
10.1.1. Extraocular Anatomy and Physiology Adapted to Retinal Detachment Treatment
10.1.2. Extraocular Anatomy and Physiology Adapted to Retinal Detachment Treatment
10.1.3. Vitreous Liquefaction
10.1.4. Posterior Vitreous Detachment
10.1.5. Abnormal Vitreous-Retinal Adhesions
10.1.6. Reticular Degeneration
10.1.7. Asymptomatic Retinal Tears
10.1.8. Examination of Retinal Detachment during Consultation Color Coding in Drawing
10.1.9. Lincoff's Laws. Methods for Locating Retinal Tears
10.2. Principles of Retinal Reapplication Surgery
10.2.1. Physiological Factors That Maintain Retinal Detachment
10.2.2. Factors That Induce Retinal Detachment
10.2.3. History of Retinal Detachment Surgery, Contributions of Jules Gonin
10.2.4. Evolution of Contemporary Surgical Techniques
10.2.5. Pre-Operative Eye Examination
10.2.6. Anesthesia in Retinal Detachment Surgery
10.2.7. Methods for Creating a Chorioretinal Adhesion
10.3. Scleral Surgery for Retinal Detachment
10.3.1. Materials for Scleral Indentation
10.3.2. Preparation of the RD's Surgical Process in the Clinic
10.3.3. Preparing the Surgical Field
10.3.4. Examination of Retinal Detachment in the Operating Theatre. Location of Tears and Their Scleral Markings
10.3.5. Sealing of Retinal Tears, Positioning of the Various Devices, Locks, Silicone Sponges, etc.
10.3.6. Cryotherapy or Laser Around Ruptures, Surgical Technique
10.3.7. Drainage and Control of Subretinal Fluid
10.3.8. Scleral Cerclage Height Adjustment and Suturing of Intraocular Implants and Injections
10.3.9. Closure and End of Surgery
10.3.10. Medical Treatment Accompanying the Scleral Surgical Process
10.4. Alternative Methods of Treatment for Retinal Detachment
10.4.1. Pneumatic Retinopexy
10.4.2. Lincoff Balloon or Orbital or Episcleral Balloon
10.4.3. Suprachoroidal Surgery, Suprachoroidal Indentation
10.4.4. Liquid-Air Exchanges in Consultation with Expanding Gases
10.4.5. Nd:YAG Laser Vitreolysis
10.4.6. Enzymatic Vitreolysis
10.5. Complicated Types of Retinal Detachment
10.5.1. Total Retinal Detachments with Multiple Retinal Tears
10.5.2. Retinal Detachments of Posterior Pole Retina Caused by Macular Holes
10.5.3. Retinal Detachment Due to Giant Tears
10.5.4. Proliferative Vitreoretinopathy
10.5.5. Retinal Detachment Secondary to Uveitis and Retinitis
10.5.6. Retinal Detachment Secondary to Choroidal Detachment
10.5.7. Retinal Detachment Secondary to Retinal Coloboma
10.5.8. Retinal Detachment Secondary to Morning Glory Syndrome
10.5.9. Retinal Detachment Secondary to Retinoschisis
10.5.10. Retinal Detachment Secondary to Anterior Segment Surgery
10.5.11. Retinal Detachment with Major Corneal Opacity
10.5.12. Retinal Detachment in the Myopic Patient
10.6. Vitrectomy for the Treatment of Retinal Detachment
10.6.1. First Steps of Current and Past Vitrectomy
10.6.2. Central and Peripheral Vitrectomy
10.6.3. Use of Liquid Perfluorocarbon
10.6.4. Surgical Techniques for Retinal Reapplication Depending on the Location of the Tear
10.6.5. Endolaser
10.6.6. Endocular Cryotherapy
10.6.7. Endocular Diathermy
10.6.8. Surgical Techniques of Intraocular Exchanges, Liquid-Air, Liquid-Oil, Liquid-Oi Silicone
10.6.9. Removal of Silicone Oil From the Anterior Chamber, Posterior Pole. Extraction of Heavy Oils
10.6.10. Control of Hemorrhage During Surgery
10.6.11. Membrane Clearance in Proliferative Vitreoretinopathy (PVR)
10.6.12. Anterior Retinectomy
10.6.13. Posterior Relaxing Retinotomy
10.6.14. Other Retinal Reapplication Techniques
10.6.15. Post-surgical Postural Treatment
10.6.16. Changes in Pressure, Aeroplane Flights During the Presence of Expandable Gases in the Eye
10.6.17. Expandable Gases and Anesthetic Gases
10.7. Complications of Retinal Detachment Surgery
10.7.1. Complications Arising from Sclerotomies
10.7.2. Retinal Incarceration at the Drainage Site in Scleral Surgery
10.7.3. All Aspects of the Lens in Retinal Detachment Surgery
10.7.4. Surgical Techniques for Mechanical Dilation of the Pupil
10.7.5. Intraoperative Complications of Retinal Detachment Surgery
10.7.6. Perioperative Complications of Retinal Detachment Surgery
10.7.7. Postoperative Complications of Retinal Detachment Surgery
Module 11. Surgery in High Myopia. Surgery in Diseases of the Macula.Surgical Techniques in Eye Trauma. Latest Surgical Techniques
11.1. Surgery for High Myopia
11.1.1. The Sclera in High Myopia
11.1.2. The Peripheral Retina in the High Myopia
11.1.3. Surgical Equipment Adapted to High Myopia
11.1.4. Vitreomacular Traction Syndrome and Epiretinal Membrane in High Myopia
11.1.5. Macular Retinoschisis
11.1.6. Myopic Macular Hole
11.1.7. Macular Indentation
11.1.8. Intraoperative Complications in High Myopia
11.1.9. Perioperative Complications in High Myopia
11.2. Vitrectomies for Macular Diseases
11.2.1. Idiopathic Macular Holes
11.2.2. Epiretinal Membranes
11.2.3. Vitreomacular Traction Syndrome
11.2.4. Colobomatous Fossa of the Optic Nerve
11.2.5. Submacular Hemorrhage
11.2.6. The Use of Tissue Plasminogen Activator in Submacular Hemorrhage Surgery
11.2.7. Submacular Surgery of Neovascular Complexes
11.2.8. Surgical Techniques for Subretinal Surgery
11.2.9. Pigment Epithelium Cell Transplantation
11.2.10. Vitrectomy in Vitreous Opacities
11.2.11. Surgical Techniques to Apply Gene Therapy
11.3. Surgical Techniques in Eye Trauma
11.3.1. Examination of Eye Injuries in the Consultation Room
11.3.2. Exploration and Primary Scleral Repair of Ocular Perforator Trauma
11.3.3. Treatment of Hyphema
11.3.4. Surgical Techniques Iridodialysis Repair
11.3.5. Surgical Techniques for the Treatment of Traumatic Lens Dislocation or Subluxation or Traumatic Intraocular Lenses
11.3.6. Surgical Techniques for Intraocular Foreign Bodies
11.3.7. Penetrating and Piercing Injuries
11.3.8. Traumatic Suprachoroidal Hemorrhages
11.3.9. Sympathetic Ophthalmia
11.4. Other Retinal Surgery Techniques
11.4.1. Surgical Techniques in Retinal Occlusion
11.4.2. Removal of Intra-Arterial Emboli
11.4.3. Terson Syndrome
11.4.4. Macular Translocation
11.4.5. Artificial Vision, Bionic Retinal Prostheses
11.4.6. Intraoperative Radiotherapy for Subretinal Neovascular Complexes
11.4.7. Surgical Techniques for the Treatment of Choroidal Detachments

A unique, key, and decisive educational experience to boost your professional development”
Master’s Degree in Macular, Retinal and Vitreous Pathology and Surgery
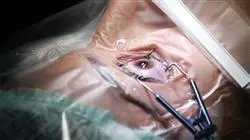
Some individuals, especially those over the age of 50, experience a particular condition in the retina that can affect their vision. This involves a tear in the central part of the retina, which, although initially asymptomatic, can lead to symptoms such as metamorphopsia, macropsia, micropsia, Watzke-Allen sign, and even severe vision loss if left untreated. This tear is known as a macular hole, and surgical intervention is required for correction. At TECH Global University, we present the Master's Degree in Macula, Retina, and Vitreous Pathology and Surgery—a comprehensive, theoretically and practically rigorous academic tool that will enable you to diagnose and address this condition and many others involving precise ocular procedures. Few educational programs offer the opportunity to delve into ophthalmology subspecialties as we do. Our fully virtual program offers the latest scientific and technological innovations in the field, providing you with cutting-edge knowledge and skills.
Aspire to be a high-performance ocular surgeon
Vitrectomy is a micro-incisional surgical technique used to replace the vitreous humor, which requires a meticulous and methodical approach. Our program not only trains you in this procedure but also in various other techniques to address pathologies such as cystoid macular edema, serpiginous choroiditis, uveitis, ocular leprosy, hereditary retinal dystrophies, albinism, and more. Supported by a team of top-level ophthalmology instructors, we will teach you how to manage intraocular hemorrhages during surgery and other complications related to retinal detachment, as well as the latest advancements in artificial vision bionic prosthetics. Our methodology is designed to provide flexible access to this content from any location and device with online connectivity, allowing you to balance your studies with other activities. Join us and discover why we are globally recognized for transforming graduates into true experts in their field.