University certificate
The world's largest faculty of medicine”
Introduction to the Program
With this Master's Degree you will delve into the latest scientific findings in circulating biomarkers and tissue molecular markers”
The life expectancy of patients with digestive system tumors has increased considerably in recent years. But where this improvement has been most noticeable is in colon tumors. Early detection, more efficient surgery and more precise treatment have been the main reasons for this progress. However, the complexity involved in managing these tumors is a challenge for medical professionals, who must keep pace with advances in surgical techniques, molecular biology and radiotherapy therapies.
This Master's Degree has been designed in response to the need for doctors to keep up to date, and is taught by a multidisciplinary teaching staff with experience in dealing with oncology patients. The program follows a syllabus that takes a theoretical-practical approach to the knowledge of new standards, the introduction of new treatments and the ability to recognize cases where it is necessary to cooperate with more complex care centers.
A program where students have at their disposal innovative educational material consisting of video summaries, detailed videos, interactive summaries so they can study molecular biology and translational oncology, digestive tract tumors, pancreatic cancer, biliary tract tumors and hepatocarcinoma in depth over the course of 12 months. What is more, the program includes practical case simulations that will prove helpful to professionals who wish to become aware of real situations and how to invervene based on the experience and knowledge of our teaching team.
TECH offers an excellent opportunity for specialists who seek to obtain quality education compatible with their work and personal responsibilities. Students only need an electronic device (computer, tablet or cell phone) to access the entire syllabus on the virtual platform. There is no need for attendance or sessions with fixed schedules, physicians can connect whenever it suits them. This flexibility is provided so that students can update their knowledge with the most agile and convenient methodology.
A high-level education designed so that professionals like you can balance their professional practice with their academic updating”
This Master's Degree in Digestive System Oncology contains the most complete and up-to-date scientific program on the market. The most important features of the program include:
- Diagnostic-therapeutic developments in the assessment, diagnosis, and intervention in Digestive System Oncology
- Contains practical exercises where the self-evaluation process can be carried out to improve learning
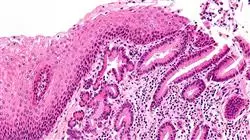
- Iconography of clinical and diagnostic imaging tests
- An algorithm-based interactive learning system for decision-making in the clinical situations presented throughout the course
- With special emphasis on evidence-based medicine and research methodologies in Digestive System Oncology
- All of this will be complemented by theoretical lessons, questions to the expert, debate forums on controversial topics, and individual reflection assignments
- Content that is accessible from any fixed or portable device with an Internet connection
The library of multimedia resources will provide contextual and situated study where learning will be much more effective”
The program’s teaching staff includes professionals from the sector who contribute their work experience to this training program, as well as renowned specialists from leading societies and prestigious universities.
The multimedia content, developed with the latest educational technology, will provide the professional with situated and contextual learning, i.e., a simulated environment that will provide immersive specialization programmed to learn in real situations.
This program is designed around Problem-Based Learning, whereby the professional must try to solve the different professional practice situations that arise throughout the program. For this purpose, the student will be assisted by an innovative interactive video system created by renowned and experienced experts.
Delve into new scientific findings on the role of the immune response in digestive cancer control with this Master's Degree"

Delve into the most effective approach to neoadjuvant and adjuvant treatment in gastric cancer with this program"
Syllabus
The Relearning system, which TECH uses in all its programs, allows professionals to progress in a much more dynamic and natural way over the course of this program. Furthermore, it is a method that favors the reduction of study time so common to other methodologies. Thanks to this, physicians will update their knowledge of advances in molecular biology, oncology and clinical management much more quickly. Likewise, being able to access this content 24 hours a day gives students greater freedom to distribute the 1,500 teaching hours the program includes.

A university education that will allow you to further develop your knowledge in palliative care patient management and the Enhanced Supportive Care integration model”
Module 1. Molecular Biology and Translational Oncology
1.1. Molecular Mechanisms of Cancer
1.2. Tumor Immunology: Basis of Cancer Immunotherapy
1.3. Role of the Biobank in Clinical Research
1.4. Understanding the New Technology: Next Generation Sequence (NGS) in Clinical Practice
1.5. Liquid Biopsies: A Trend or the Future?
1.6. Update on Molecular Markers for Treatment Decisions in Gastrointestinal Malignancies
1.7. Do Molecular and Immunological Classifications Have Clinical Implications Today?
Module 2. Upper Gastrointestinal Tract Tumors
2.1. Esophageal Cancer
2.1.1. Differences between Squamous Carcinoma and Esophagus Adenocarcinoma
2.1.2. Endoscopic Aspects of Esophageal Cancer: Diagnosis and Staging
2.1.3. Clinical Impact of 18F-FDG PET/CT in the Therapeutic Management of Patients with Esophageal Cancer
2.1.4. Endoscopic Treatment of Superficial Esophageal Neoplasms
2.1.5. Conventional Surgical Approach to Esophageal Carcinoma
2.1.6. Minimally Invasive and Robotic Surgery of Esophageal Cancer
2.1.7. Evolution in Neoadjuvant and Adjuvant Treatment of Esophageal Cancer
2.1.8. Management of Metastatic Esophageal Cancer
2.2. Gastric Cancer
2.2.1. Diagnosis and Staging of Gastric Adenocarcinoma
2.2.2. Minimally Invasive and Robotic Surgery of Gastric Cancer
2.2.3. Lymphadenectomy Extension in Gastric Cancer
2.2.4. Neoadjuvant and Adjuvant Treatment in Gastric Cancer: What Is the Optimal Approach?
2.2.5. First-Line Treatment of HER2-Negative Metastatic Gastric Cancer
2.2.6. Second-Line Treatment of HER2-Negative Metastatic Gastric Cancer
2.2.7. Metastatic Gastric Cancer: Impact of Drugs Targeting the HER2 Pathway
2.2.8. Metastatic Gastric Cancer: Impact of Immune Checkpoint Inhibitors
Module 3. Lower Gastrointestinal Tract Tumors
3.1. Colon and Rectum Cancer
3.1.1. Colorectal Cancer: Epidemiology, Etiology and Incidence
3.1.2. Molecular Mechanisms Involved in the Invasion and Metastasis Process in Digestive Tumors
3.1.3. Molecular Classification of Colon Cancer: New Perspectives
3.1.4. Biomarkers in Colorectal Cancer
3.1.5. Early Detection Program for Colon and Rectum Cancer
3.1.6. Familial Forms of Colorectal Cancer (Polyposis-Associated and Non-Polyposis-Associated)
3.1.7. Cancer Associated with Chronic Inflammatory Bowel Diseases and Treatments Received
3.1.8. Diagnosis and Endoscopic Management of Polyps and Advanced Lesions
3.1.9. Clinical Impact of FDG-PET/CT in the Staging of Colorectal Cancer
3.1.10. Role of Endoscopic Ultrasonography (EUS) and Magnetic Resonance Imaging (MRI) in the Staging of Rectal Cancer
3.1.11. Laparoscopic vs. Robotic Surgery in Colon Cancer
3.1.12. Surgical Management of Familial Non-Polyposis Colon Cancer
3.1.13. Surgery for Familial Adenomatous Polyposis
3.1.14. Current Adjuvant Treatment of Colon Cancer and Proposals for the Future in the Adjuvant Treatment of Colon Cancer
3.1.15. Total Mesorectal Excision: Open, Laparoscopic and Robotic
3.1.16. Transanal Approach to Rectal Tumors
3.1.17. Neoadjuvant Treatment in Rectal Cancer
3.1.18. Postoperative Treatment after Neoadjuvant and Radical Surgery
3.1.19. Observe and Wait for Low Rectal Cancers after Neoadjuvant Therapy with Complete Clinical Response
3.1.20. Invasive Pelvic Tumors: Pelvic Exenteration
3.1.21. Therapeutic Advances in Colon and Rectal Cancer: Improving Patient Survival Day by Day
3.1.22. What Is the Best Treatment Option After Second Line Therapy in Advanced Colorectal Cancer?
3.1.23. Acquired Resistance to EGFR Antibodies: How to Manage
3.1.24. Immunotherapy in Metastatic Colorectal Cancer
3.1.25. Rectal Cancer with Synchronous and Resectable Liver Metastases
3.1.26. Management of Colorectal Cancer Liver Metastases
3.1.27. Total Mesocolon Excision: When? How? Why?
3.1.28. Role of Endoscopy in the Management of Advanced Colorectal Cancer
Module 4. Other Digestive Tract Tumors
4.1. Appendicular Tumors
4.1.1. Appendicular Tumors: Surgical Implications
4.2. Peritoneal Carcinomatosis
4.2.1. Peritoneal Carcinomatosis: Surgical Treatment and Postoperative Intraperitoneal Chemotherapy
4.3. Anal Cancer
4.3.1. Treatment of Localized Anal Cancer
4.3.2. Treatment of Locally Advanced Cancer
4.3.3. Treatment of Radiation Therapy in Colon Cancer
4.3.4. Treatment of Metastatic Anal Cancer
4.4. Neuroendocrine Tumors
4.4.1. Neuroendocrine Tumors of the Small Intestine
4.4.2. Neuroendocrine Tumors of the Pancreas
4.4.3. Surgical Treatment of Non-Functioning Neuroendocrine Pancreas Tumors
4.4.4. Surgical Treatment of Gastrinoma
4.4.5. Surgical Treatment of Insulinoma
4.4.6. Pancreas Endocrine Tumors Surgery: Glucagonoma, Vipoma
4.4.7. Overview of Systemic Treatment of Metastatic Neuroendocrine Tumors in the Pancreatic Gastroenteropancreatic Tract
4.5. GIST
4.5.1. Biology, Diagnosis and Management of Gastrointestinal Stromal Tumors (GIST)
4.5.2. The Role of 18F-FDG PET/CT in GI Stromal Tumors
4.5.3. Surgical Treatment of Gastrointestinal Stromal Tumors (GIST)
4.5.4. GIST as a Model of Translational Research: 15 Years of Experience
4.6. Lymphomas
4.6.1. Gastric MALT Lymphoma
4.6.2. Lymphomas in Other Digestive Regions
Module 5. Pancreatic Cancer, Biliary Tract Tumors and Hepatocarcinoma
5.1. Pancreatic Cancer
5.1.1. Epidemiology, Risk Factors and Diagnosis of Pancreatic Cancer
5.1.2. Use of Endoscopic Retrograde Cholangiopancreatography (ERCP) in Patients with Pancreatic Masses and Biliary Tract Obstruction
5.1.3. Use of Endoscopic Ultrasonography (EUS) in Pancreatic Cancer Patients or Pancreatic Masses
5.1.4. Endosonographic Cholangiopancreatography (CEPEUS) in Pancreatic Masses and Biliary Tract Obstruction
5.1.5. Diagnostic Modalities for Defining Pancreatic Cancer Resectability (CT, EUS, MRI)
5.1.6. Clinical Impact of PET/CT with 18F-FDG in the Therapeutic Management of Patients with Pancreas Cancer
5.1.7. Borderline Resectable Pancreatic Cancer
5.1.8. Laparoscopic Distal Pancreatectomy: Indications and Technique
5.1.9. Cephalic Pylorus-Preserving Duodenopancreatectomy vs. Whipple in Pancreatic Cancer
5.1.10. Surgical Treatment of Ampulomas
5.1.11. Adjuvant and Neoadjuvant Chemotherapy Treatment for Pancreatic Cancer
5.1.12. Adjuvant and Neoadjuvant Radiotherapy Treatment for Pancreatic Cancer
5.1.13. Advances in the Treatment of Patients with Metastatic Pancreatic Cancer
5.1.14. Screening for Familial and Hereditary Pancreatic Cancer
5.1.15. Cystic Lesions of the Pancreas of Neoplastic Origin
5.1.16. Surgery for Cystic Tumors of the Pancreas
5.2. Cholangiocarcinoma and Gallbladder Cancer
5.2.1. Epidemiology, Risk Factors and Diagnosis of Cholangiocarcinoma and Gallbladder Cancer
5.2.2. What to Do with Cholangiocarcinoma
5.2.3. Advances in the Treatment of Patients with Metastatic Cholangiocarcinoma and Gallbladder Cancer
5.3. Hepatocellular Carcinoma
5.3.1. Epidemiology, Risk Factors and Diagnoses for Hepatocellular Carcinoma
5.3.2. Staging and Treatment of Hepatocellular Carcinoma
5.3.3. Resective Treatment vs. Liver Transplantation in Hepatocellular Carcinoma
5.3.4. Locally Advanced Disease with Vascular Involvement Local Therapy vs. Systemic Therapy
5.3.5. Drainage of Malignant Biliary Obstruction by Interventional Radiology
5.3.6. First and Second Line of Systemic Therapy in Hepatocellular Carcinoma
5.3.7. Recurrence of Hepatocellular Carcinoma after Transplantation
Module 6. Collaboration in the Management of Oncology Patients
6.1. Palliative Management
6.1.1. The Palliative Care Consultant in the Multidisciplinary Team: “Planning Treatments”
6.1.2. A Model of Integration with Oncology: Enhanced Supportive Care
6.1.3. Informed Consent: Are We Really Informing Our Patients?
6.1.4. Palliative Management of Symptoms in Gastrointestinal Tumors
6.1.5. Palliative Endoscopic Treatments
6.1.6. Palliative Surgical Treatment
6.2. Emergencies and Comorbidities
6.2.1. Why do Patients with Gastrointestinal Tumors Attend the Emergency Department and How Can Outcomes Be Improved?
6.2.2. Infectious Comorbidity Management
6.2.3. Cardiovascular Comorbidity Management
6.2.4. Neurologic Comorbidity Management
6.2.5. Endocrinological Comorbidity Management
6.2.6. Nutritional Comorbidity Management
6.2.7. Gastrointestinal Tumors in the Elderly
6.2.8. Outpatient Care of Patients with Digestive System Oncology Pathology
Module 7. From Clinical Management to Networking
7.1. Clinical Management in Digestive Tumor Units
7.1.1. Principles of Clinical Management
7.1.2. Intensified Recovery Programs in Colon Surgery
7.1.3. Members, Functions and Decision-Making in Multidisciplinary Teams
7.2. Improving Networking
7.2.1. Technological Platforms for Patient Monitoring and Control
7.2.2. The Collaborative Online World
7.2.3. Decision Support Systems in Oncology Based on Artificial Intelligence

A unique, key, and decisive training experience to boost your professional development”
Master's Degree in Digestive System Oncology
The Master's Degree in Digestive System Oncology is an academic program designed for medical professionals who wish to specialize in the diagnosis and treatment of digestive cancers. This program provides comprehensive and up-to-date training in the latest techniques and advancements in the research and treatment of cancers such as esophageal, gastric, liver, pancreatic, small intestine, colon, and rectal cancer. Digestive oncology is a constantly evolving discipline due to ongoing research into the mechanisms that trigger cancer. The Master's Degree in Digestive System Oncology at TECH Global University focuses on providing integrated training in the various areas involved in digestive oncology, such as surgery, medical oncology, radiotherapy, and clinical research. This master's program aims to offer rigorous research in the prevention, early detection, diagnosis, and treatment of different types of digestive cancers. Additionally, it seeks to enable professionals to evaluate and follow up with patients suffering from these conditions, providing comprehensive and personalized treatment.
Study 100% online and take your career to the next level
The Master's Degree in Digestive System Oncology covers current and relevant topics such as epidemiology, biomarkers, molecular diagnostics, and imaging techniques, as well as advances in surgery, radiotherapy, and chemotherapy. Special attention is also given to ethical and legal aspects in oncological care. The program is aimed at specialist physicians in gastroenterology, oncology, surgery, radiotherapy, and other medical disciplines related to digestive oncology. It is also suitable for professionals in digestive diseases with an interest in oncology research. This Master's Degree in Digestive System Oncology offers complete and up-to-date training in the latest techniques and advances in the research and treatment of various types of digestive cancers, providing medical professionals with the highest quality specialization. At TECH, we offer real-world examples to solve, which will challenge you as you study with us. Don’t miss the opportunity to advance your career with a top-tier education.







